Antihistamine Safety Checker
Antihistamine Safety Assessment
Find out if your antihistamine is safe for your blood pressure condition.
When you're battling allergies, antihistamines can be a lifeline. But if you have high blood pressure, a simple over-the-counter pill might not be as harmless as it seems. Many people assume all antihistamines are safe - but that’s not true. Some can lower your blood pressure. Others, especially when mixed with decongestants, can push it dangerously high. The key isn’t avoiding antihistamines altogether. It’s knowing which ones to use, when to monitor, and what to watch for.
How Antihistamines Actually Affect Blood Pressure
Antihistamines work by blocking histamine, a chemical your body releases during allergic reactions. Histamine makes blood vessels expand and leak fluid - that’s why your nose runs and your skin swells. By blocking histamine’s action, antihistamines reduce those symptoms. But histamine also plays a role in keeping your blood vessels tense and your blood pressure stable. When you block it, you can disrupt that balance.First-generation antihistamines like diphenhydramine (Benadryl) are the biggest concern. They cross the blood-brain barrier easily and have strong effects on blood vessels. Studies show that when given intravenously, diphenhydramine can drop systolic blood pressure by 8-12 mmHg within 15 minutes. Even taken orally, some people report dizziness or lightheadedness - signs of mild hypotension. This isn’t just anecdotal. A Drugs.com review of 1,200 users found 14% reported dizziness upon standing, a classic sign of orthostatic hypotension.
Second-generation antihistamines like loratadine (Claritin), cetirizine (Zyrtec), and fexofenadine (Allegra) are different. They barely enter the brain and don’t interfere much with blood vessel tone. The FDA reviewed over 50 clinical trials through 2022 and found loratadine had no meaningful effect on blood pressure in 97% of cases. Cetirizine even showed potential benefits in animal studies, reducing heart inflammation by 33%. For most people with high blood pressure, these are the safest choices.
The Real Danger: Combination Products
The biggest risk isn’t from antihistamines alone. It’s from combo pills - the ones labeled for "sinus relief," "allergy and congestion," or "nighttime allergy." These almost always include a decongestant like pseudoephedrine or phenylephrine.Pseudoephedrine is a stimulant. It tightens blood vessels to reduce nasal swelling - but it also raises blood pressure. GoodRx’s 2023 analysis of 12 clinical trials found that pseudoephedrine increases systolic blood pressure by about 1 mmHg on average. Sounds small? Not when you’re already hypertensive. In a group of 4,328 patients surveyed, nearly half reported their blood pressure rising 5-10 mmHg after using these combo products. That’s enough to undo months of controlled treatment.
Other common combinations carry risks too. Products with ibuprofen can raise blood pressure by 3-4 mmHg. Those with acetaminophen can push it up by up to 5 mmHg - especially if taken at the maximum daily dose of 4,000 mg. And because these are sold as "all-in-one" solutions, many people don’t realize they’re getting a hidden blood pressure trigger.
Who’s at Risk? Who’s Safe?
Not everyone needs to avoid antihistamines. But some people should be extra careful.If you have:
- Uncontrolled high blood pressure (systolic above 140 mmHg)
- Heart disease, arrhythmias, or a history of stroke
- Are taking multiple blood pressure medications
- Have liver problems or take drugs like ketoconazole or erythromycin
-then you need to choose wisely. Stick to second-generation antihistamines. Avoid anything with pseudoephedrine, phenylephrine, or other decongestants. Skip diphenhydramine unless it’s an emergency.
For most people with well-controlled hypertension, second-generation antihistamines are safe. A 2022 survey by the American Academy of Allergy found 92% of hypertensive patients using cetirizine reported no blood pressure changes. The same study showed 68% of users on loratadine had no issues. These aren’t just lab results - they’re real-world experiences from people living with both allergies and high blood pressure.
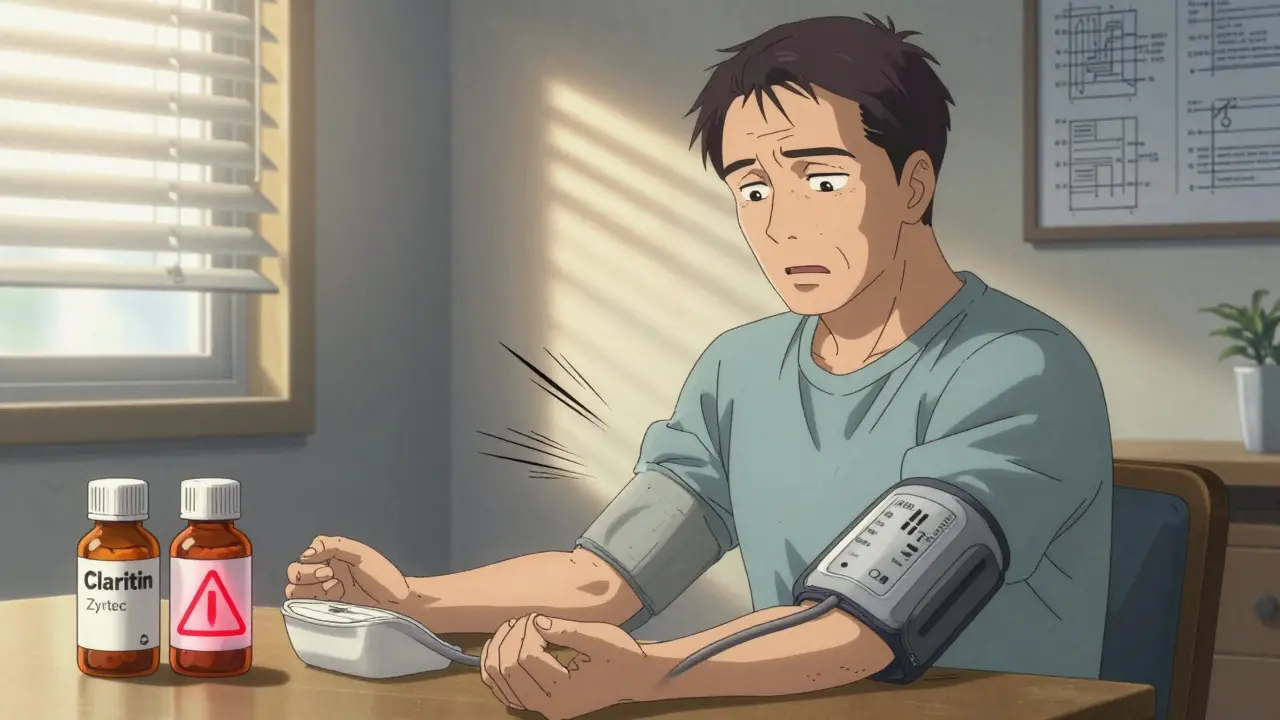
Monitoring Your Blood Pressure: Simple Steps
You don’t need a doctor’s office visit every time you take an antihistamine. But you do need a plan.Here’s what the American Heart Association recommends for people with hypertension:
- Check your blood pressure before your first dose of any new antihistamine.
- If you’re using diphenhydramine or another first-generation drug, check again 30-60 minutes after taking it.
- If you’re using a second-generation antihistamine without decongestants, no extra monitoring is needed - unless you feel dizzy, lightheaded, or your usual symptoms worsen.
- If you’re using a combo product with pseudoephedrine, check your blood pressure 2-4 hours after the first dose.
- Keep a log: Write down your readings for 3 days before and after starting the medication.
Use a validated home blood pressure monitor. Wrist and finger devices are less accurate. Upper arm cuffs are best. Many pharmacies sell them for under $30. A few weeks of tracking can tell you whether a new allergy med is helping or hurting your heart.
What to Avoid Completely
Some antihistamines were pulled from the market for a reason. Terfenadine (Seldane) and astemizole (Hismanal) were withdrawn in 1999 after causing deadly heart rhythm problems. They blocked potassium channels in the heart, leading to long QT syndrome and sudden cardiac arrest.Even though they’re gone, you might still hear them mentioned online. Don’t be fooled. Don’t buy old stock. Don’t trust unregulated online sellers. These drugs are banned for good reason.
Also avoid promethazine (Phenergan) if you have heart issues. It’s a first-generation antihistamine with strong sedative effects and documented links to low blood pressure and arrhythmias. It’s still used in hospitals, but not for routine allergy relief.
What to Choose Instead
If you have high blood pressure and allergies, here’s your simple guide:- Best choice: Fexofenadine (Allegra) - least likely to interact with other meds, no liver metabolism issues.
- Very good choice: Loratadine (Claritin) - neutral effect on blood pressure, widely studied.
- Good choice: Cetirizine (Zyrtec) - slightly more sedating but safe for most with hypertension.
- Avoid: Diphenhydramine (Benadryl), chlorpheniramine, promethazine - unless under direct medical supervision.
- Never use: Any product with pseudoephedrine, phenylephrine, or other decongestants unless your doctor says it’s safe.
Check the active ingredients on the label. If it says "Plus," "Sinus," "Nighttime," or "Multi-Symptom," assume it has a decongestant. Look for "non-drowsy" or "allergy only" - those are usually safer.
When to Call Your Doctor
You don’t need to panic every time you take an antihistamine. But call your doctor if you notice:- Systolic blood pressure rising more than 10 mmHg above your usual baseline
- Dizziness, fainting, or feeling like you might pass out
- Heart palpitations or irregular heartbeat
- Swelling in your ankles or sudden shortness of breath
These aren’t normal side effects. They could mean your blood pressure is reacting badly - or worse, you’re having an allergic reaction that’s stressing your heart.
Also, if you’re taking other medications - especially for heart disease, depression, or infections - talk to your pharmacist. Some drugs interact with antihistamines and raise the risk of side effects. Grapefruit juice, for example, can increase levels of certain antihistamines in your blood, leading to unexpected drops in pressure or heart rhythm issues.
The Future: Safer Allergy Treatments
Science is moving fast. Researchers are now studying how genetic differences affect how people respond to antihistamines. Some people metabolize these drugs slowly due to variations in the CYP2D6 or CYP3A4 enzymes. That means even a standard dose could build up and cause problems.By 2023, 32% of major U.S. healthcare systems started offering genetic testing for high-risk patients before prescribing antihistamines. This isn’t routine yet - but it’s coming.
There’s also exciting new research on selective H3 receptor agonists. Early studies suggest they could calm allergic reactions without affecting blood pressure at all. Phase I trials began in late 2023. These won’t be available for years, but they point to a future where allergy relief doesn’t come with a cardiovascular trade-off.
For now, stick with what works: second-generation antihistamines, no decongestants, and smart monitoring. You don’t have to suffer through allergy season. You just need to choose the right tool for your body.
Can antihistamines raise blood pressure?
Pure antihistamines like loratadine, cetirizine, and fexofenadine do not raise blood pressure in most people. However, combination products that include decongestants like pseudoephedrine can increase systolic blood pressure by 5-10 mmHg. Always check the active ingredients on the label.
Is Benadryl safe if I have high blood pressure?
Diphenhydramine (Benadryl) can cause a drop in blood pressure, especially when given intravenously or in higher doses. It may also cause dizziness and lightheadedness. For people with high blood pressure, it’s not the first choice. Second-generation antihistamines like Claritin or Zyrtec are safer and just as effective for most allergy symptoms.
Which antihistamine is safest for people with hypertension?
Fexofenadine (Allegra) is considered the safest because it has minimal interaction with liver enzymes and doesn’t affect blood pressure. Loratadine (Claritin) and cetirizine (Zyrtec) are also safe options for most people with controlled hypertension. Avoid any product with pseudoephedrine or other decongestants.
Can I take antihistamines with my blood pressure medication?
Second-generation antihistamines like loratadine and fexofenadine rarely interact with blood pressure medications. But always check with your pharmacist or doctor, especially if you’re taking drugs like ketoconazole, erythromycin, or certain antidepressants. These can interfere with how your body breaks down antihistamines and increase side effects.
Do I need to monitor my blood pressure when starting an antihistamine?
Yes - if you have high blood pressure, check your pressure before your first dose. If you’re taking a first-generation antihistamine like diphenhydramine, check again 30-60 minutes later. For second-generation antihistamines without decongestants, monitoring isn’t usually needed unless you feel dizzy or your usual symptoms worsen.

Comments
swarnima singh
so i just took benadryl for my sneezing and now i feel like i’m floating?? like is this normal or am i just weak?? my bp was 130/85 before, now it’s 110/70 and i’m kinda scared but also weirdly calm?? idk man.
Ryan Hutchison
Look, if you’re in America and you’re taking anything with pseudoephedrine and you’re hypertensive, you’re basically playing Russian roulette with your heart. The FDA doesn’t care. Big Pharma doesn’t care. But I care. I’ve seen guys in the VA hospital with BP spikes from those "allergy + sinus" pills. Don’t be that guy. Read the label. Or don’t. But don’t come crying when your stroke happens.
Samyak Shertok
Oh wow, so we’re now treating allergies like a nuclear threat? 🤡
"Avoid diphenhydramine unless it’s an emergency" - what emergency? Your nose is running? You’re not dying. You’re just… sniffing. Meanwhile, the real crisis is that we’ve turned a simple histamine response into a 12-page medical thriller with graphs and FDA reviews. Can we just… breathe? Or is that too much to ask without a blood pressure monitor and a pharmacist on speed dial?
Stephen Tulloch
Allegra > Claritin > Zyrtec - no debate. 🧠💯
Also, if you’re using a wrist BP monitor, you’re already losing. Go buy a $25 Omron. I’m not even mad. I’m just disappointed. And yes, I’ve done the 3-day log thing. It’s boring as hell, but it saved my life after I took that "Nighttime Allergy Relief" crap. Don’t be a hero. Track it. 📊❤️
Melodie Lesesne
This was so helpful!! I’ve been taking Zyrtec for years and never thought twice - now I’m checking the label every time I grab a box. Also, I just got my first home BP cuff and I’m weirdly proud of myself 😊
Thanks for breaking it down so clearly - I feel way less scared now!
Chelsea Harton
benadryl drops bp? i thought it made you sleepy not dizzy
Corey Chrisinger
It’s wild how we treat allergies like they’re just a nuisance - but they’re actually a window into how fragile our autonomic nervous system is. Histamine isn’t just about runny noses. It’s a signaling molecule that connects immune response, vascular tone, even sleep. We block it like it’s a bug… but we’re not just fixing a symptom. We’re tinkering with a system that’s been evolving for 500 million years.
And now we’re surprised when it glitches? 🤔
Maybe the real question isn’t "which antihistamine?" - but "why do we keep trying to fix nature with pills?"
Bianca Leonhardt
People still take Benadryl? Like… really? You’re 30 and you think OTC meds are harmless? You’re lucky you haven’t ended up in the ER. Stop being lazy. Get a prescription. Or just suffer through spring. Your heart will thank you. 🙄
Travis Craw
thanks for the info. i’ve been using claritin for years and never had issues. just wanted to say i appreciate how you laid out the risks without scaring people. i’ll keep checking labels. and yeah, i got the arm cuff too. it’s kinda satisfying to see the numbers go down 😅