Benzodiazepine Interaction Risk Checker
Check Your Medication Risk
This tool assesses the risk of combining benzodiazepines with other substances based on FDA warnings and medical research. The combination of benzodiazepines with opioids or alcohol can be fatal.
Please select your medications and click "Check Risk Level" to see your risk assessment.
When anxiety hits hard, a doctor might reach for a benzodiazepine-something like Xanax, Ativan, or Valium-to bring calm fast. These drugs work in minutes, not weeks, making them tempting for panic attacks, severe stress, or sleepless nights. But here’s the part no one tells you until it’s too late: benzodiazepines aren’t just about anxiety relief. They’re a silent partner in deadly combinations with other common medications.
How Benzodiazepines Actually Work
Benzodiazepines boost the effect of GABA, your brain’s natural calming chemical. That’s why they reduce anxiety, relax muscles, and sometimes knock you out. But that same mechanism makes them dangerous when paired with other depressants. Think of your nervous system like a car’s brakes. Benzodiazepines press the pedal. Opioids? They press harder. Alcohol? That’s stomping the pedal down with both feet. These drugs come in three flavors based on how long they last in your body:- Short-acting: Alprazolam (Xanax), triazolam (Halcion) - 6 to 12 hours. These are the ones people use for panic attacks. But they wear off fast, leading to rebound anxiety and a higher risk of dependence.
- Intermediate-acting: Lorazepam (Ativan) - 10 to 20 hours. Often used in hospitals for acute anxiety or before surgery.
- Long-acting: Diazepam (Valium), clonazepam (Klonopin) - up to 100 hours. Built up in the system over time, which can be helpful for some, but makes withdrawal harder.
The Deadly Mix: Benzodiazepines and Opioids
This is where things turn deadly. Between 2011 and 2016, 75% of all benzodiazepine-related overdose deaths involved opioids. That’s not a coincidence. It’s a pattern. When you take both, your breathing slows down-so much that your body forgets to breathe at all. The FDA found that people using both drugs together had a 15 times higher risk of fatal overdose than those taking opioids alone. A 2017 study in JAMA Internal Medicine showed patients on both opioids and benzodiazepines had a 154% higher chance of overdose than those on opioids only. And it’s not just street drugs. Many people are prescribed both: painkillers like oxycodone or hydrocodone for chronic pain, and Xanax or Ativan for anxiety. That’s not rare. A 2022 survey by the Anxiety and Depression Association of America found 32% of benzodiazepine users were also taking opioids. One Reddit user, u/AnxietyWarrior2020, shared: “I was on oxycodone for back pain and Xanax for panic attacks. Two weeks in, I stopped breathing during sleep. Woke up in the ER with oxygen tubes up my nose.” That’s not an outlier. It’s a warning.Alcohol? Don’t Even Think About It
Alcohol and benzodiazepines? That’s a classic combo people think is harmless. “I just had a glass of wine,” they say. But that “glass” can turn your calm into a coma. Both depress the central nervous system. Together, they can cause extreme drowsiness, loss of coordination, vomiting, and respiratory failure. A 2023 Healthgrades analysis of 1,247 patient reviews showed 27% of negative experiences mentioned dangerous interactions-with alcohol being the top offender. One review said: “I had one drink while on Ativan. I blacked out and woke up on the floor. My husband called 911.” The FDA now requires every benzodiazepine prescription to include a Boxed Warning-its strongest safety alert-stating clearly: “Combining with alcohol can cause death.” That warning didn’t exist in 2010. It’s here now because too many people died.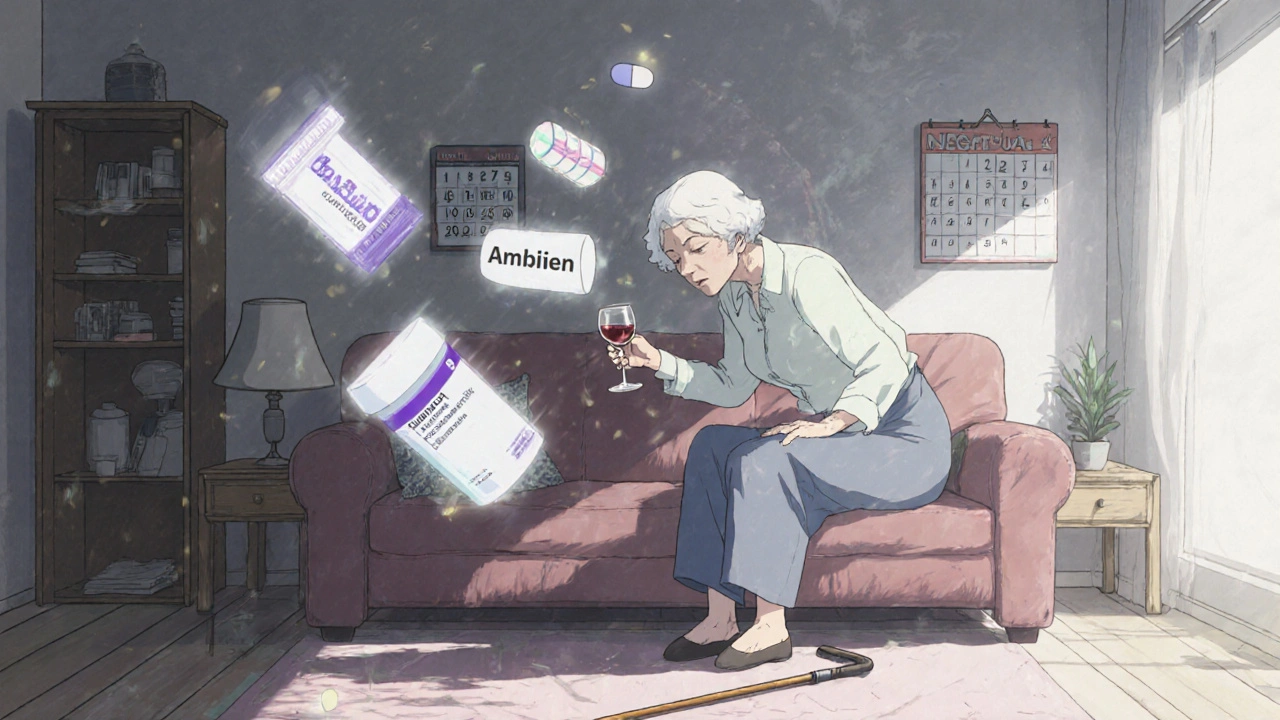
Older Adults Are at Higher Risk
For people over 65, benzodiazepines are a fall waiting to happen. These drugs slow reaction time, blur vision, and mess with balance. The American Geriatrics Society’s Beers Criteria says: Don’t prescribe these to older adults unless there’s no other option. The risk of falling and breaking a hip jumps by 50% just from taking a benzodiazepine alone. Add another sedating drug-like a sleep aid, muscle relaxant, or even an antihistamine for allergies-and that risk triples. In 2019, a study in the Journal of the American Geriatrics Society found that seniors on multiple sedating drugs were far more likely to end up in the hospital from a fall. And it’s not just physical. Benzodiazepines can fog thinking, worsen memory, and mimic dementia. Many older patients are misdiagnosed with Alzheimer’s when they’re just on Valium for “nerves.”What About Other Anxiety Meds?
There are safer long-term options. SSRIs like sertraline (Zoloft) or escitalopram (Lexapro) take 4 to 6 weeks to kick in, but they don’t cause dependence, don’t interact dangerously with alcohol or painkillers, and work well for most anxiety disorders. They’re now the first-line treatment for new anxiety diagnoses, prescribed in 68% of cases compared to just 22% for benzodiazepines. Buspirone is another alternative. It doesn’t sedate you. It doesn’t cause withdrawal. It doesn’t interact badly with other meds. But it’s slow. It’s not for panic attacks. It’s for daily anxiety that builds slowly. Z-drugs like zolpidem (Ambien) are often seen as “safer” benzodiazepine alternatives for sleep. But they’re not. They still depress the CNS. They still carry overdose risks when mixed with opioids or alcohol. And they’re just as addictive.
When Are Benzodiazepines Actually Okay?
They’re not all bad. Used right, they can save lives. A patient recovering from major surgery might need a few days of Ativan to manage terror-induced insomnia. Someone in acute alcohol withdrawal might need Valium to prevent seizures. A panic attack during a flight? A single dose of Xanax can make the difference between a meltdown and a calm arrival. The key is: short-term. No longer than 2 to 4 weeks. And never, ever with opioids or alcohol. Dr. Christine Musso from Hartford Hospital puts it plainly: “When used appropriately for short-term crises, benzodiazepines can be life-saving.” But that’s the phrase everyone forgets: short-term.What Should You Do?
If you’re on a benzodiazepine:- Ask your doctor: Are you also on an opioid, sleep aid, muscle relaxant, or alcohol? If yes, get a safety plan now.
- Never stop cold turkey. Withdrawal from benzodiazepines can cause seizures, hallucinations, or death. Tapering must be slow and supervised.
- Use a pill tracker. Apps like Medisafe or even a simple paper log help you spot dangerous combos before they happen.
- Know your pharmacy’s alerts. Many pharmacies now flag dangerous interactions. If they don’t, ask them to.
- Ask about alternatives. If you’ve been on benzodiazepines for more than a month, it’s time to talk about switching to an SSRI or therapy.
The Bigger Picture
The U.S. benzodiazepine market is shrinking. Prescriptions dropped from 13.1% of adults in 2013 to 10.8% in 2021. Why? Because people are waking up. States with prescription drug monitoring programs that alert doctors about opioid-benzo combos saw a 27% drop in dangerous pairings within 18 months. Medicare now requires special paperwork before approving both drugs together. The message is clear: benzodiazepines have a role, but it’s narrow. They’re not for daily anxiety. They’re not for long-term use. And they’re absolutely not for mixing with other depressants. The FDA didn’t update their warnings because they wanted to. They did it because people were dying. And they’re still dying-every day.Can I take benzodiazepines with over-the-counter sleep aids?
No. Most over-the-counter sleep aids like diphenhydramine (Benadryl, Tylenol PM) or doxylamine (Unisom) are antihistamines that cause drowsiness. Mixing them with benzodiazepines can lead to extreme sedation, confusion, slowed breathing, and even coma. Even if the label says "natural" or "herbal," if it makes you sleepy, it’s unsafe with Xanax, Ativan, or Valium.
Is it safe to drink alcohol occasionally while on benzodiazepines?
No. There is no safe amount. Even one drink can double the sedative effect of a benzodiazepine. This isn’t about getting drunk-it’s about your brain forgetting to control your breathing. The FDA’s Boxed Warning explicitly states this combination can be fatal. There’s no exception for "just one glass" or "only on weekends."
How do I know if I’m dependent on benzodiazepines?
If you’ve taken them daily for more than 2 weeks and feel anxious, shaky, or have trouble sleeping when you miss a dose, you’re likely dependent. Other signs: needing higher doses to get the same effect, or feeling like you can’t function without them. Dependence isn’t addiction-it’s your body adapting. But it still requires medical help to taper safely. Don’t try to quit cold turkey.
Are there safer alternatives for long-term anxiety?
Yes. SSRIs like sertraline or escitalopram are the first choice for long-term anxiety management. They take 4-6 weeks to work but have no abuse potential and minimal interaction risks. Therapy-especially CBT-is just as effective and has lasting results. Buspirone is another non-addictive option, though it’s slower and less effective for panic attacks.
What should I do if I’m already taking benzodiazepines and opioids?
Don’t stop either one on your own. Contact your doctor immediately. This combination is extremely dangerous. Your doctor may refer you to a pain specialist or addiction specialist to safely reduce one or both medications. Many hospitals now have programs specifically for patients on this dangerous combo. The goal isn’t to take you off all meds-it’s to get you off the deadly mix.


Comments
Jessica Healey
I took Xanax for like 3 months after my dad died. Thought it was a gift from heaven. Then I realized I couldn’t sleep without it, and my anxiety got worse when I wasn’t on it. I cried for two days straight when I tried to quit. Never again. SSRIs sucked at first, but now I’m actually living, not just surviving.
Joseph Peel
The data here is solid. The FDA’s boxed warning didn’t appear out of thin air. It appeared because doctors kept prescribing benzos like candy while patients were on opioids, and then they stopped breathing. We need better prescriber education, not just patient warnings.
Kelsey Robertson
Oh, please. ‘Short-term use only’? That’s what they said about opioids too… and look where that got us. You’re just swapping one addiction for another-SSRIs don’t ‘work’ for most people, they just dull the pain until you forget you’re alive. And therapy? That’s for people who can afford 150 bucks an hour and have the emotional stamina to relive their trauma on a couch. Meanwhile, my Valium lets me drive my kids to school without hyperventilating. Don’t shame me for functional survival.
Joseph Townsend
Y’all are acting like benzos are the devil’s cough syrup. I’ve seen people on them for 10 years and they’re still running marathons, raising kids, and running businesses. Meanwhile, SSRIs turn people into walking zombies who can’t feel joy, love, or even pizza. And don’t get me started on ‘therapy’-it’s just a glorified chat with someone who charges by the minute while you’re still stuck in your head. I’ll take my Ativan and my wine, thank you very much. I’m not dying because I want to feel okay.
Bill Machi
Let’s be clear: this isn’t about medical advice. It’s about cultural decay. We’ve turned every emotional discomfort into a pharmaceutical problem. You’re anxious? Take a pill. Can’t sleep? Take a pill. Feeling overwhelmed? Take two. We’ve outsourced resilience to Big Pharma, and now we’re surprised when people overdose on their own helplessness. Stop medicating your way out of life’s hard parts. Build discipline. Learn to breathe. It’s not that complicated.
Elia DOnald Maluleke
Respectfully, the West has turned suffering into a commodity. In my country, elders sit with pain. They do not rush to chemically silence it. Benzodiazepines are not a solution-they are an escape, and escape is not healing. The body remembers what the mind tries to forget. I have seen men in Johannesburg, after losing jobs and families, take these pills-and then vanish into silence. No one asks why they are hurting. They only ask how to make it stop.
satya pradeep
Bro, I was on Klonopin for 8 months after my mom passed. I didn’t know I was dependent until I tried to stop and my hands shook like I had Parkinson’s. My doc didn’t warn me. Pharmacy didn’t flag it. I almost had a seizure. Now I’m on Zoloft + weekly therapy. It’s slow as hell but I actually feel like ME again. Don’t wait till your body betrays you. Talk to someone before it’s too late.
Prem Hungry
Dear friend, I understand your pain. Please know you are not alone. Many have walked this path before you. The journey to healing is not always fast, but it is always worth it. Consider speaking with a licensed counselor, and if possible, ask your physician about non-addictive alternatives like buspirone or mindfulness-based cognitive therapy. You deserve peace without dependency. Take one step today. You are stronger than you think.
Leslie Douglas-Churchwell
EVERYTHING HERE IS A LIE. 🤫 The FDA? Controlled by Big Pharma. SSRIs? Designed to keep you docile and working. The ‘danger’ of benzos? A distraction so they can push antidepressants that cost $200/month and come with 14 side effects including suicidal ideation. And don’t get me started on ‘therapy’-that’s just brainwashing with a clipboard. They want you addicted to the system, not the pills. The real danger? Trusting anyone who says ‘short-term use.’ They’re all in on it. 💊👁️🗨️
shubham seth
Let’s cut the BS. You’re all pretending this is about safety. It’s about control. Pharma doesn’t care if you live or die-they care if you keep buying. SSRIs? Still patented. Benzos? Generic. Cheaper to kill you with a $0.10 pill than to fund a 5-year CBT program. The ‘warning labels’? PR spin. The real solution? Ban all psych meds. Let people suffer. Maybe then we’ll fix the damn system instead of drugging the symptoms.
Kathryn Ware
I just want to say-this post saved my life. I was on Xanax for 3 years, drinking wine every night, and taking Unisom because I thought I needed help sleeping. I didn’t realize I was basically poisoning myself. I went to my doctor and said, ‘I think I’m addicted.’ She didn’t judge me. We made a plan. I’m 8 weeks into tapering, on Lexapro, and going to CBT twice a week. I still have bad days. But now I’m not hiding. I’m healing. And if you’re reading this and you’re scared? You’re not alone. Ask for help. It’s not weak. It’s the bravest thing you’ll ever do. 💛