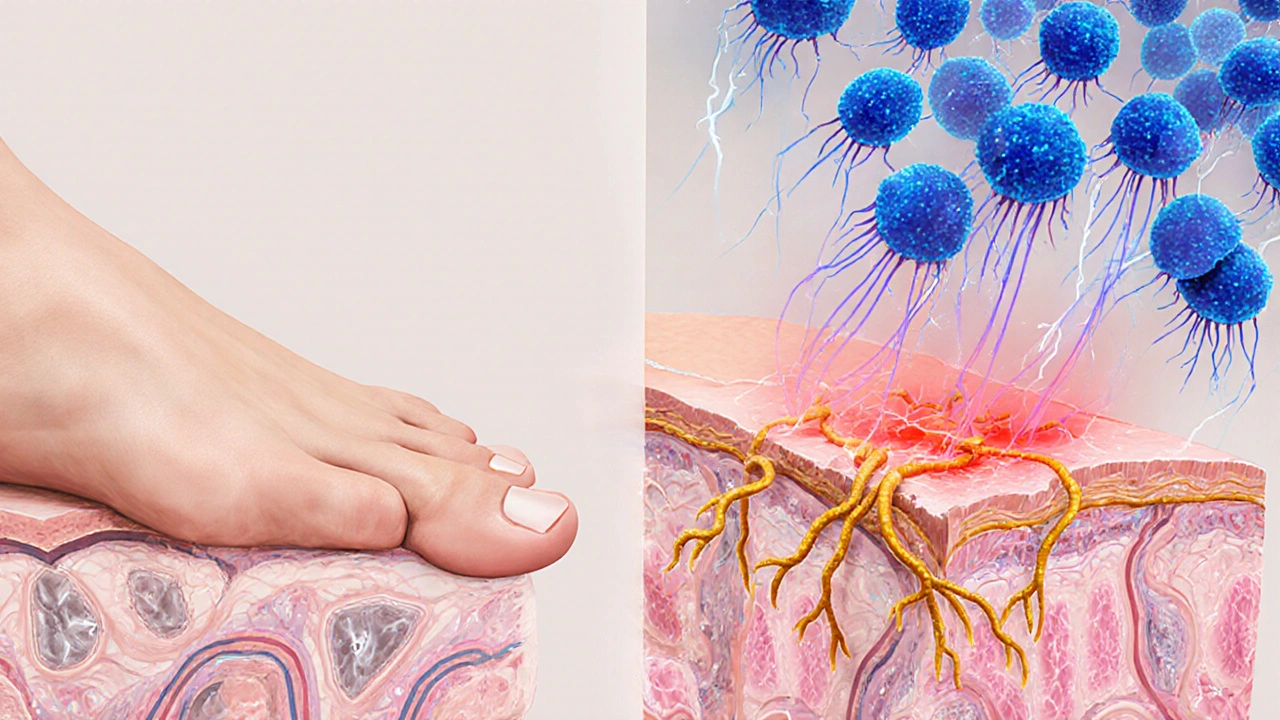
When you notice itching, burning, or peeling skin between your toes, athlete's foot is likely the culprit. Athlete's foot is a common fungal infection of the feet caused primarily by dermatophyte fungi, affecting the skin’s keratin‑rich areas such as the toes and soles. While many treat it as a simple nuisance, the condition can actually reveal a lot about how well your immune system is functioning. Below we’ll explore how athlete’s foot and immune health intersect, what that means for everyday people, and practical steps to keep both your skin and immunity in top shape.
What Causes Athlete’s Foot?
Understanding the root of the problem starts with the fungal players. Dermatophyte fungi are a group of keratin‑feeding organisms, including Trichophyton rubrum and Epidermophyton floccosum, that thrive in warm, damp environments like locker rooms, public showers, and sweaty shoes. These microbes cling to the skin’s outer layer, exploiting any cracks or moisture to grow.
The infection usually begins when spores land on a compromised skin barrier. Factors that weaken this barrier-such as excessive sweating, tight footwear, or existing skin conditions-make it easier for the fungi to take hold.
Immune System Basics: The Body’s Defense Network
Before linking the two, let’s quickly recap the immune system’s role. Immune system is a complex network of cells, tissues, and organs that protects the body from infections, cancers, and other harmful agents includes innate components (like skin, mucous membranes, and white blood cells) and adaptive components (T cells, B cells, antibodies). Among adaptive cells, T cells are a type of lymphocyte that recognize and destroy infected cells, orchestrate other immune responses, and generate memory for future protection play a critical role in identifying fungal invaders.
When any part of this system is weakened-whether by chronic disease, medication, or lifestyle-the body’s ability to keep opportunistic organisms like dermatophytes in check diminishes.
How Immune Health Influences Athlete’s Foot Risk
Research consistently shows that individuals with compromised immunity face a higher incidence and severity of fungal foot infections. Here are the most common scenarios where the immune system’s performance directly impacts foot health:
- Diabetes: Elevated blood sugar can impair neutrophil function and reduce circulation, creating a perfect breeding ground for fungi.
- HIV/AIDS: Reduced CD4+ T‑cell counts blunt the adaptive response, allowing infections to spread more aggressively.
- Immunosuppressive drugs: Corticosteroids, chemotherapy, and biologics dampen both innate and adaptive immunity, increasing the odds of persistent athlete’s foot.
- Age‑related immunity decline: Elderly individuals often experience slower skin turnover and weakened cell‑mediated immunity.
In these groups, athlete’s foot is not just a mild irritation; it can become chronic, spread to the nails (tinea unguium), or even cause secondary bacterial infections.
Can Athlete’s Foot Weaken Your Immune System?
The relationship is not one‑way. A persistent fungal infection can tax the immune system, especially if it triggers ongoing inflammation. Chronic inflammation releases cytokines that, over time, may lead to immune dysregulation. Moreover, the skin barrier’s integrity is crucial; when breached, it can become a portal for other pathogens, increasing overall infection risk.
For most healthy adults, a typical bout of athlete’s foot won’t dramatically affect systemic immunity. However, people already battling other inflammatory conditions (like eczema or psoriasis) might notice a flare‑up in overall symptoms because the immune system is already on high alert.
Key Risk Factors Beyond Immunity
While immune health is a major piece, other factors also dictate susceptibility. Below is a quick checklist many overlook:
- Wearing non‑breathable shoes for extended periods.
- Sharing towels, socks, or footwear in public spaces.
- Having damp feet for more than 10 minutes a day (e.g., after swimming).
- Existing skin conditions like athlete’s foot’s cousin, jock itch.
- Neglecting foot hygiene: not drying between toes.
Addressing these habits often prevents infection even when immune defenses are modest.
Treatment Options: From Topical to Systemic
The good news is that athlete’s foot is highly treatable. The choice of therapy depends on infection severity, recurrence, and the patient’s immune status.
- Topical antifungals: Over‑the‑counter creams, sprays, or powders containing terbinafine, clotrimazole, or miconazole are effective for mild cases.
- Oral antifungal medication: For extensive or recurrent disease, doctors may prescribe terbinafine or itraconazole tablets, especially for immunocompromised patients.
- Adjunct hygiene measures: Keeping feet dry, rotating shoes, and using antifungal powders in socks can boost treatment success.
When treating someone with a weakened immune system, clinicians often combine topical and oral agents and monitor liver function, as systemic antifungals can have hepatic side effects.
Preventive Strategies to Support Both Skin and Immunity
Prevention works best when it tackles the fungal source and bolsters overall immune resilience. Follow these evidence‑backed steps:
- Maintain dry feet: After bathing, thoroughly towel dry, especially between digits. Consider using a hair dryer on cool setting.
- Choose breathable footwear: Opt for shoes made of leather or mesh; avoid plastic clogs.
- Use antifungal powder: Sprinkle in shoes and socks, especially if you sweat heavily.
- Rotate shoes: Give each pair at least 24hours to air out.
- Boost immune health: Eat a diet rich in vitaminsC andD, zinc, and probiotic foods; get regular moderate exercise and adequate sleep.
- Manage underlying conditions: Keep blood sugar under control if diabetic, and stay on schedule with HIV medication or other chronic disease treatments.
- Avoid sharing personal items: Towels, socks, and footwear should be personal.
These measures create a hostile environment for dermatophytes while giving your immune system the energy it needs to stay vigilant.

When to Seek Medical Help
If you notice any of the following, it’s time to see a healthcare professional:
- Symptoms persisting beyond two weeks despite OTC treatment.
- Severe redness, swelling, or pus - signs of secondary bacterial infection.
- Spread to nails, hands, or groin.
- Repeated episodes (more than three per year).
- Existing immune‑compromising conditions (diabetes, HIV, transplant, chemotherapy).
Early intervention can prevent chronic infection and limit any extra strain on your immune system.
Quick Reference Table
| Risk Factor | Immune‑Competent Individuals | Immune‑Compromised Individuals |
|---|---|---|
| Warm, moist environment | Occasional infection; usually resolves with OTC treatment | Higher chance of chronic infection; may need prescription meds |
| Diabetes | Increased risk; monitor closely | Significant risk; rapid progression, possible complications |
| Immunosuppressive therapy | Not applicable | Frequent recurrences; systemic treatment often required |
| Poor foot hygiene | Can trigger infection | Exacerbates existing vulnerability |
Bottom Line
Athlete’s foot isn’t just a superficial annoyance; it can serve as a window into your immune health. By understanding the fungal biology, recognizing how immune deficits raise infection risk, and adopting both treatment and preventive habits, you can keep your feet comfortable and your immune system robust.
Frequently Asked Questions
Can athlete’s foot spread to other parts of the body?
Yes. The fungi that cause athlete’s foot can travel to the hands, groin (jock itch), or nails, especially if you scratch the infected area and then touch other skin surfaces.
Is it safe to use over‑the‑counter antifungal creams if I have diabetes?
Generally, yes. Start with a topical agent and monitor healing. If the infection doesn’t improve in two weeks, consult a doctor for possible oral therapy.
How long does it take for athlete’s foot to clear up?
With proper topical treatment, most mild cases resolve within 1-2 weeks. More stubborn or widespread infections may require 4-6 weeks of therapy.
Do antifungal powders help prevent infection?
Yes. Powders absorb moisture and can inhibit fungal growth, making them a useful adjunct to shoes and socks, especially for athletes or people who sweat heavily.
Can a weak immune system cause more severe itching?
A weakened immune response may allow the fungus to proliferate faster, leading to larger patches and more intense itching compared with someone who clears the infection quickly.


Comments
Allison Marruffo
I’ve seen quite a few athletes neglect basic foot hygiene, assuming a quick rinse is enough. Consistently drying between the toes and rotating shoes can dramatically cut down fungal growth. Pairing those habits with a diet rich in vitamin D and zinc supports immune defenses. When the skin barrier stays intact, dermatophytes have little foothold to exploit. Keeping these simple steps in mind can make a big difference.
Ian Frith
Imagine stepping out onto the court only to feel that unmistakable burning between your toes-like a tiny inferno under your skin. That sensation isn’t just a nuisance; it’s your body’s alarm that the immune system is being challenged. The fungi thrive in the damp shadows of sweaty shoes, waiting for any slip in immunity. Even a modest dip in T‑cell activity can tip the scales toward infection. So treat athlete’s foot as a clue, not a footnote, in your overall health story.
Beauty & Nail Care dublin2
I swear, the moment I put on my new kicks, my feet started itching like mad 😂. Who knew a simple pair of shoes could turn into a fungal playground? Keep those toes dry, use powder, and maybe don’t share socks at the gym 🙈. Trust me, the itchier it gets, the more you’ll wish you’d listened sooner! 🌟
Oliver Harvey
Well, that’s just fantastic.
Ben Poulson
In light of the presented information, it is evident that proper foot care constitutes a paramount factor in preventing dermatophytic infections. The correlation between immunocompetence and susceptibility to such conditions warrants meticulous attention. Accordingly, individuals should integrate rigorous hygiene practices with regular medical consultations. Such a comprehensive approach is likely to mitigate the incidence of athlete’s foot. Your consideration of these recommendations is appreciated.
Raghav Narayan
The interplay between cutaneous immunity and fungal colonisation is a subject that has intrigued clinicians for decades.
Keratinised epidermal layers serve as both a physical barricade and a medium through which immune cells can surveil for invading pathogens.
When the integrity of this barrier is compromised-by excessive moisture, micro‑trauma, or occlusive footwear-dermatophytes gain a foothold.
At the same time, innate immune components such as Langerhans cells and neutrophils are mobilised to recognise fungal antigens.
These cells release cytokines that orchestrate an inflammatory response aimed at containing the infection.
In immunocompetent hosts, this cascade typically resolves the infection within a week or two, especially when aided by topical antifungals.
However, in individuals with diabetes, HIV, or those receiving corticosteroids, the efficacy of this response diminishes markedly.
Reduced neutrophil chemotaxis and impaired T‑cell mediated immunity allow the fungus to proliferate unchecked.
Consequently, lesions may enlarge, become hyperkeratotic, and even spread to the nails or other body sites.
Chronic infection further perpetuates a cycle of low‑grade inflammation, which can subtly skew systemic immune regulation.
This persistent inflammatory milieu may interfere with the body’s ability to respond to unrelated pathogens.
Therefore, addressing athlete’s foot in such patients is not merely a matter of comfort but a component of holistic immune management.
Preventive strategies should combine rigorous foot hygiene, moisture‑wicking materials, and, when appropriate, prophylactic antifungal powders.
Additionally, optimisation of systemic health-through glycaemic control, adequate nutrition, and regular exercise-strengthens overall immune resilience.
In summary, the management of athlete’s foot offers a valuable window into the broader health of the host, and clinicians should treat it with the seriousness it deserves.
Tara Phillips
It is advisable to adopt a regimented foot‑care routine, encompassing thorough drying and the use of breathable footwear. Complementary to these measures, periodic application of antifungal agents can preempt recurrence. Moreover, maintaining a balanced diet rich in micronutrients fortifies systemic immunity. Such diligence not only alleviates the immediate discomfort but also safeguards long‑term health. Your commitment to these protocols is commendable.
Derrick Blount
One might argue, dear readers, that the very act of neglecting foot hygiene is a microcosm of modern complacency, a symptom, perhaps, of a society too hurried to notice the subtle warnings of our own bodies; indeed, the fungal spores do not merely linger, they exploit, they proliferate, they admonish us, and they persist until we intervene, wisely, decisively, with both topical remedies and disciplined daily habits.
Anna Graf
Keep your feet dry and change socks often. Use powder if your feet get sweaty. This helps stop the fungus.
Jarrod Benson
Hey folks, let’s get real about those nasty toe rashes-stop ignoring them! When you’re hitting the gym or the field, your shoes get hot and wet, and that’s a perfect party for fungus. A quick tip: after every workout, give your shoes a break, toss them in the sun, and splash a little antifungal spray inside. Also, invest in socks that breathe, because soggy socks are basically a fungal five‑star hotel. Trust me, a few small changes now will save you weeks of itching later, and you’ll be back to crushing your goals without that annoying distraction.
Liz .
Foot care is key and just a few simple steps can keep fungus away you just need to dry your toes and wear good shoes
tom tatomi
Actually, it’s far from great-it underscores how easily we overlook fundamental health basics :)
Tom Haymes
Consistent foot hygiene paired with regular check‑ins from a healthcare provider creates a strong defense against recurring infections. When you treat the skin barrier as part of your overall fitness regimen, you’ll notice fewer flare‑ups. Keep tracking your progress, and adjust your routine as needed.
Scott Kohler
One would presume that the general populace, inundated with medical literature, would already recognise the triviality of neglecting foot sanitation; alas, the persistence of athlete’s foot serves as a testament to our collective superficiality.
Brittany McGuigan
Our nation’s health depends on disciplined habits, and ignoring foot fungus is simply unacceptable.
Priya Vadivel
It can be incredibly frustrating, especially when you’re juggling multiple health concerns, but remember, every step you take toward better foot care-drying thoroughly, choosing breathable footwear, using antifungal powder-contributes to a stronger immune system, and you deserve all the support on this journey.
Dharmraj Kevat
Feet burn like hell when you ignore the signs
Lindy Fujimoto
Oh dear, the tiny fungi are plotting a rebellion on your toes, but fear not-armed with powder, fresh socks, and a splash of confidence, you shall vanquish them! 🌟💪
darren coen
Dry feet, breathable shoes, repeat.
Jennifer Boyd
Keep up the great work on your foot health-each small habit builds a fortress against fungus, and you’re doing amazing!