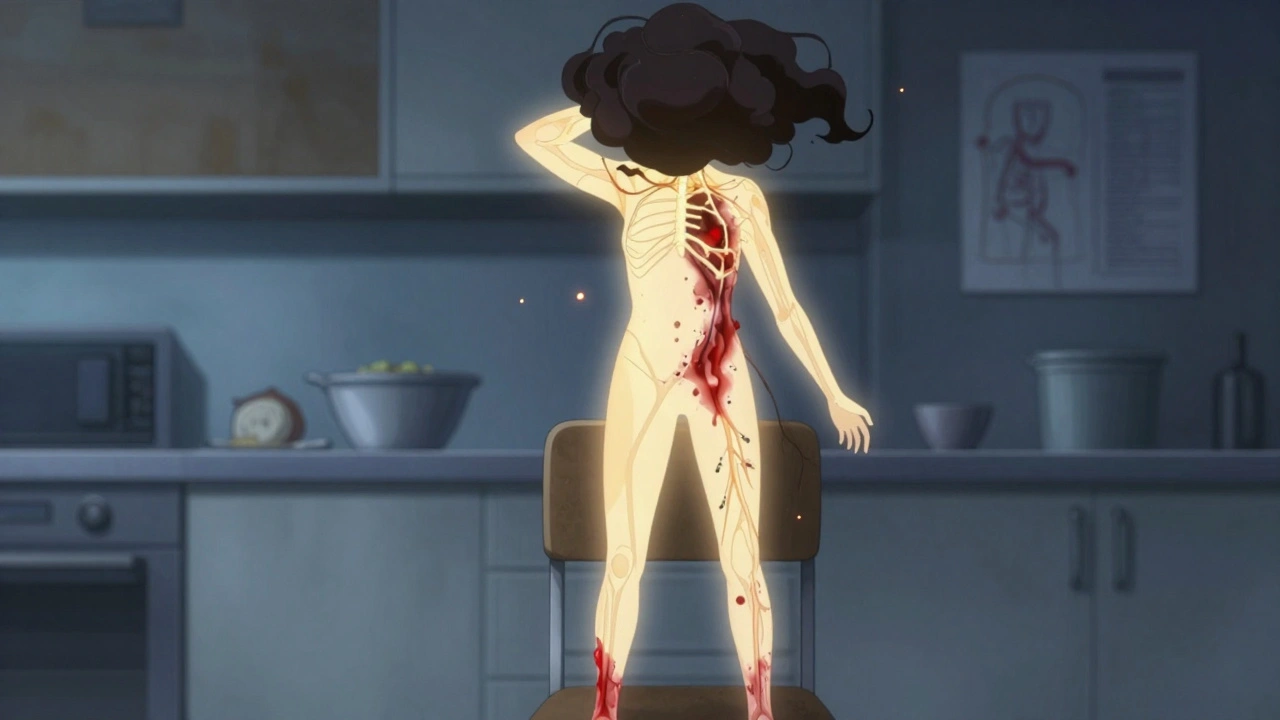
When you stand up from a chair, your body should automatically adjust-blood vessels tighten, heart rate increases slightly, and blood pressure stays steady so your brain doesn’t go dark. But for people with autonomic neuropathy, that automatic response breaks down. The result? Sudden dizziness, blurred vision, or even fainting. And it’s not just about standing up. Digestion becomes a nightmare-nausea, vomiting, bloating, constipation, or unpredictable diarrhea. This isn’t just inconvenience. It’s a serious neurological condition that silently damages the nerves controlling your heart, blood pressure, and gut.
What Exactly Is Autonomic Neuropathy?
Autonomic neuropathy is nerve damage that affects the autonomic nervous system-the part of your nerves that runs things you don’t think about: heartbeat, digestion, sweating, bladder control, and blood pressure. It’s most commonly linked to long-term diabetes. About 85-90% of cases happen in people with diabetes who’ve had high blood sugar for years. High glucose and fat levels slowly poison the tiny blood vessels that feed these nerves, causing them to misfire or die off.
But it’s not just diabetes. Autoimmune disorders, certain chemotherapy drugs like vincristine, viral infections like Guillain-Barré, and even Parkinson’s disease can trigger it. The problem? Most people don’t know they have it until symptoms get bad. Studies show only about 30% of primary care doctors recognize the signs early. That means many patients suffer for years before getting a proper diagnosis-on average, 4.7 years.
Why Your Blood Pressure Plummets When You Stand
One of the most dangerous and common symptoms is orthostatic hypotension-your blood pressure drops too much when you stand. The definition? A systolic drop of 20 mmHg or more, or a diastolic drop of 10 mmHg or more, within three minutes of standing. In severe cases, systolic pressure can crash from 120 to 85 in under 30 seconds.
This happens because the damaged nerves can’t signal blood vessels to squeeze tight when you stand. Blood pools in your legs instead of returning to your heart and brain. That’s why people feel lightheaded, see spots, or pass out. About 30% of people with diabetic autonomic neuropathy experience this. In a 2021 study of 450 patients, 68% had symptomatic low blood pressure during standing tests, and 42% had episodes at least once a week.
Some people develop POTS-Postural Orthostatic Tachycardia Syndrome-instead. Here, blood pressure doesn’t drop much, but the heart races-by 30 beats per minute or more-just from standing. It’s common in young women and often mistaken for anxiety. But it’s neurological. Heart rate variability tests, tilt-table tests, and deep breathing tests are used to confirm it.
How Your Gut Turns Against You
While blood pressure issues grab attention, gastrointestinal symptoms are just as disabling-and often more embarrassing. Up to 55% of people with autonomic neuropathy have gut problems. The most common is gastroparesis: your stomach stops emptying properly. Food sits there for hours. That leads to bloating, early fullness, nausea, and vomiting-especially at night. In one study, 78% of gastroparesis patients with autonomic damage vomited nightly.
Constipation is equally common, affecting 60% of patients. Bowel movements drop from the normal 4-5 times a week to just 1-2. But then, paradoxically, diarrhea hits-often at night. Why? The gut’s rhythm is broken. Food moves too slowly in some areas, too fast in others. This creates the perfect environment for small intestinal bacterial overgrowth (SIBO), which shows up in 52% of these patients versus 15% in healthy people. SIBO causes gas, bloating, and watery stools.
Swallowing can also become hard. Esophageal motility tests show 40-60% of patients have weak contractions in the esophagus. That means food sticks, and people feel like something’s lodged in their throat.

How Doctors Diagnose It
There’s no single blood test. Diagnosis relies on a mix of symptoms and objective tests. The simplest? The 10-minute active stand test. You lie down for 5 minutes, then stand. Blood pressure and heart rate are measured at 1, 3, 5, and 10 minutes. A drop of 20 mmHg systolic or 10 mmHg diastolic confirms orthostatic hypotension.
For heart function, doctors use heart rate variability during deep breathing. A normal ratio between exhale and inhale is above 1.1. Below that? Nerve damage. The Valsalva maneuver-forcing air out against a closed airway-tests how well your body recovers pressure. And for the gut, gastric emptying scintigraphy is still the gold standard: you eat a meal with a tiny radioactive tracer, and a camera tracks how fast it leaves your stomach. If more than 10% is still there after 4 hours, it’s gastroparesis.
Questionnaires like COMPASS-31 help too. It scores symptoms from 0 to 100. A score above 30 means significant autonomic dysfunction. Studies show it matches objective tests 85% of the time.
Treatment: What Actually Works
There’s no cure, but symptoms can be managed. For low blood pressure, fludrocortisone helps by making your body hold onto salt and water. But it can cause high blood pressure when lying down-35% of users get this side effect. Midodrine tightens blood vessels and helps 70% of people, but it must be taken 3-4 times a day, and you can’t take it before bed, or you’ll wake up with dangerously high pressure.
For POTS, ivabradine slows the heart without lowering blood pressure. It cuts heart rate by 15-25 bpm in 65% of users. It’s not a cure, but it gives people back hours of upright time.
For the gut, metoclopramide is often prescribed first-it speeds up stomach emptying. But after 12 weeks, it can cause permanent muscle spasms (tardive dyskinesia), so doctors avoid long-term use. Erythromycin works well short-term, but the body gets used to it fast-70% lose the effect in 2-4 weeks.
Pyridostigmine is gaining favor. It’s an old drug, originally for myasthenia gravis, but it improves gastric motility with fewer side effects. In a 2023 trial, 55% of patients saw better digestion.
Lifestyle Changes That Make a Real Difference
Medications help, but lifestyle tweaks often do more. Eating six small meals a day instead of three big ones cuts nausea and vomiting by 50% in 60% of gastroparesis patients. Avoiding fat and fiber helps too-fat slows digestion, and fiber adds bulk your stomach can’t handle. A diet with less than 25g of fat and 10g of fiber daily is recommended.
Compression stockings (30-40 mmHg) and abdominal binders reduce blood pooling in the legs and belly. One 2022 Mayo Clinic trial showed they cut orthostatic symptoms by 35-40%. Increasing salt intake (with doctor approval) and drinking 2-3 liters of water daily helps maintain blood volume.
Patients also avoid heat-showers, saunas, hot weather-because heat dilates blood vessels and makes blood pressure crash worse. Many report needing to sit down after walking just a few steps. A 2022 survey found 89% avoid hot environments, 76% wear compression gear daily, and 68% add salt to meals.

What Patients Are Saying
On Reddit’s r/dysautonomia, users describe life-changing moments. One wrote: “My BP dropped from 120/80 to 85/55 the second I stood. Fludrocortisone gave me four hours of upright time for the first time in years.” Another said: “The low-fat, low-residue diet cut my vomiting from five times a day to once every three days. Worth giving up restaurants.”
But the emotional toll is heavy. 62% say dietary restrictions ruined social life. 55% avoid eating out because they can’t predict when they’ll get sick. “Brain fog” during low-blood-pressure episodes is common-people feel mentally foggy, confused, or unable to focus.
What’s Coming Next
Research is moving fast. A new NIH trial is testing fecal transplants for GI symptoms-early results show 40% improvement in quality of life. Blood tests measuring neurofilament light chain-a protein released when nerves break down-are now being studied as early warning signs. Levels correlate strongly with symptom severity.
By 2024, the American Diabetes Association will recommend annual autonomic screening for anyone with diabetes longer than 7 years. That could catch 500,000 new cases early. In 2025, the threshold for diagnosing orthostatic hypotension may drop from 20 mmHg to 15 mmHg, helping identify milder cases before they cause falls or heart problems.
But the reality remains: autonomic neuropathy still cuts life expectancy by over 8 years in severe cases. It’s not just a side effect of diabetes-it’s a major driver of early death. The more we recognize the signs-dizziness on standing, vomiting at night, unexplained constipation-the sooner we can help people live longer, better lives.
Can autonomic neuropathy be reversed?
In most cases, nerve damage from autonomic neuropathy is permanent. But early intervention can stop it from getting worse. Tight blood sugar control in diabetics, removing toxic triggers like certain chemo drugs, and treating autoimmune causes can stabilize the condition. Some mild cases show partial recovery over years with strict management, but full reversal is rare.
Is orthostatic hypotension the same as POTS?
No. Orthostatic hypotension means your blood pressure drops too much when standing. POTS means your blood pressure stays mostly normal, but your heart rate spikes by 30 beats per minute or more. Both are forms of autonomic failure, but they’re different mechanisms. Some people have both. POTS is more common in younger women, while orthostatic hypotension is more typical in older diabetics.
Why does gastroparesis cause both constipation and diarrhea?
The nerves controlling your gut are damaged, so movement becomes chaotic. Food moves too slowly in the stomach and upper intestine, causing constipation and bloating. But in the lower gut, nerves fire randomly, leading to spasms and rapid transit-resulting in diarrhea. This alternating pattern is classic. SIBO, which often develops in this setting, makes diarrhea worse.
Can compression stockings help with dizziness when standing?
Yes. Compression stockings (30-40 mmHg) squeeze your legs and prevent blood from pooling when you stand. This helps maintain blood flow to your brain, reducing dizziness and fainting. Studies show they cut orthostatic symptoms by 35%. Many patients wear them daily and report being able to stand longer and walk farther without passing out.
What should I do if I suspect I have autonomic neuropathy?
Start by tracking your symptoms: when do you feel dizzy? How often do you vomit or have bowel changes? Note if symptoms happen after meals or when standing. See your doctor and ask for an active stand test and a COMPASS-31 questionnaire. If your primary care provider isn’t familiar, ask for a referral to a neurologist or autonomic specialist. Don’t wait-early diagnosis means better outcomes.
Next Steps If You’re Affected
If you’re dealing with unexplained dizziness on standing, vomiting at night, or bowel problems that don’t respond to usual treatments, don’t dismiss them as “just aging” or “stress.” Write down your symptoms-timing, triggers, frequency. Bring them to your doctor with a list of questions. Ask specifically about autonomic neuropathy, especially if you have diabetes, a history of chemotherapy, or an autoimmune condition.
Join a patient community. Reddit’s r/dysautonomia and MyAutonomicNeuropathy.com have thousands of people sharing what works. You’re not alone. And if you’re on medication, track your response. Did midodrine help? Did pyridostigmine reduce vomiting? That data helps your doctor adjust your plan.
Most importantly, protect yourself from falls. Use a cane if needed. Sit on the edge of the bed for a minute before standing. Avoid standing still for long periods. Wear compression gear. Drink water. Eat small meals. These aren’t just tips-they’re lifesavers.

Comments
Ruth Witte
OMG I JUST FOUND OUT I HAVE THIS 😭 I thought I was just "clumsy" or "anxious"... but after 3 years of passing out in the grocery store, my neurologist finally said it: autonomic neuropathy. Compression socks + salt + small meals = my new religion. 🙏
Noah Raines
Yea this is real. I’ve had it since my diabetes diagnosis 8 years ago. Fludrocortisone made me feel like a balloon, but midodrine? Game changer. Just don’t take it after 4pm or you’ll be wide awake at 3am with your heart pounding like a drum. Worth it.
Katherine Rodgers
so like... is this just diabetes being lazy? like why do we even call it a "neuropathy" if it's just because you didn't control your sugar? also why is everyone suddenly so dramatic about vomiting at night??
Mona Schmidt
Thank you for writing this with such clarity. I'm a nurse and I see so many patients dismissed as 'just old' or 'anxious.' This condition is underdiagnosed because the symptoms are invisible. The COMPASS-31 tool is underutilized - every diabetic over 5 years should get screened. Early detection saves lives. Please share this with your doctor.
Guylaine Lapointe
I'm sorry, but I find it irresponsible to promote "eating salt" and "compression stockings" as solutions without mentioning the risk of hypertension, edema, and venous thrombosis. This reads like a wellness blog, not medical advice. People with heart failure or renal disease shouldn't be told to chug water and salt like it's a detox.
Andrea Petrov
I know what this really is. It's not diabetes. It's not chemo. It's the 5G towers. They interfere with nerve signaling. I've been tracking my symptoms since 2020 - every time I move near a cell tower, my BP drops. The FDA knows. They just don't want you to know. Look up "neurological EMF sensitivity" - it's been suppressed for decades.
Suzanne Johnston
It's fascinating how the body's autonomic system - this invisible orchestra of involuntary functions - can be so delicately balanced, and yet so easily shattered. We treat the symptoms, but what are we really doing? Are we managing disease... or just delaying the inevitable unraveling of a system we barely understand? There's humility in that.
Graham Abbas
I used to think I was just tired. Then I fainted in the shower. Twice. Now I wear compression leggings like they're fashion. I drink 3 liters of water a day. I eat like a bird. And honestly? I feel more alive than I have in 10 years. This isn't just medicine - it's a whole new way of being. I wish I'd known sooner.
Haley P Law
I just found out I have this and I'm crying. Not because I'm sick - because I finally have a name for why I can't go to parties, why I pass out after walking to the mailbox, why I can't eat anything that smells good anymore. I'm not lazy. I'm not dramatic. I'm just broken. And now I know how to fix it.
Andrea DeWinter
Gastroparesis is the worst. The bloating feels like a balloon in your stomach. The vomiting at night? Terrifying. Pyridostigmine helped me more than anything. And low fat low fiber diet? Non negotiable. Avoid fiber like it's poison. Your gut will thank you. Also drink water. Always. Even if you don't feel like it
Steve Sullivan
I used to think POTS was just anxiety. Then I did the tilt table test and my HR went from 72 to 138 in 2 seconds. I thought I was having a panic attack. Turns out my nerves were just broken. Now I take ivabradine. It’s not magic, but it lets me stand in line at the grocery store without seeing stars. Also - compression socks. Buy them. Now.
George Taylor
I'm just... honestly... overwhelmed. Every single sentence here is a symptom I've had for years. And now I see it all laid out like a textbook. But who cares? No one listens. My PCP said "it's just stress." My mom says I'm "making it up." And now I'm reading this and realizing... I'm not crazy. I'm just chronically, invisibly, catastrophically broken. And nobody gives a damn.