Not all beta-blockers are the same. If you’ve been prescribed one, you might assume they all work the same way-lower heart rate, reduce blood pressure, calm the heart. But the truth is, choosing the right beta-blocker isn’t just about following a checklist. It’s about matching the drug’s unique properties to your body, your conditions, and your risks. Some can make breathing harder. Others might help your sex life. A few can actually reverse heart damage. The differences aren’t subtle-they change outcomes.
What Beta-Blockers Actually Do
Beta-blockers stop adrenaline and noradrenaline from binding to beta receptors in your heart and blood vessels. These chemicals are what make your heart race during stress, exercise, or panic. By blocking them, beta-blockers slow your heart rate, reduce how hard your heart pumps, and lower blood pressure. That’s why they’re used after heart attacks, for heart failure, irregular rhythms, and even migraines.
But here’s the catch: your body has three types of beta receptors. Beta-1 is mostly in the heart. Beta-2 is in your lungs, blood vessels, and muscles. Beta-3 is in fat tissue and the heart lining. Older beta-blockers hit all of them. Newer ones are pickier. And that selectivity changes everything.
First-Generation: The Broad-Spectrum Options
Propranolol was the first beta-blocker ever made. It blocks both beta-1 and beta-2 receptors equally. That’s why it works for tremors, anxiety, and migraines-it affects more than just the heart. But that also means it can cause trouble.
If you have asthma or COPD, propranolol can tighten your airways. Studies show a 20-30% higher risk of bronchospasm compared to selective agents. It can also make your hands and feet cold by constricting blood vessels. Many patients report fatigue, depression, or trouble sleeping. On Drugs.com, users give it a 6.2 out of 10. About 38% say side effects are moderate to severe.
It’s still used, but mostly when other options won’t work-like for performance anxiety or certain arrhythmias. It’s cheap, generic, and effective for some. But it’s not the go-to anymore for heart failure or high blood pressure.
Second-Generation: The Heart-Selective Ones
These drugs-atenolol, metoprolol, bisoprolol-are designed to target only beta-1 receptors. That means less impact on your lungs and blood vessels. For people with asthma or diabetes, this is a big deal. You’re less likely to have breathing problems or hidden low blood sugar.
Metoprolol comes in two forms: tartrate (Lopressor) and succinate (Toprol XL). Tartrate needs two doses a day. Succinate is once daily and better for heart failure. The extended-release version gives steadier levels, fewer side effects, and better adherence. A Cleveland Clinic survey found 85% of heart failure patients stuck with succinate because it was easier to take and caused fewer respiratory issues.
Bisoprolol is even more selective than metoprolol. It’s often preferred in older adults because it’s cleared mostly by the kidneys, not the liver. That means fewer drug interactions. Patients rate it 7.1 out of 10-higher than propranolol. Side effects like fatigue and cold extremities are lower, too.
Atenolol is the oldest of this group. It’s cheap, but studies show it doesn’t reduce heart attack risk as well as others in heart failure. It’s also less effective at lowering central aortic pressure, which matters for long-term heart health. Many cardiologists avoid it for heart failure now.
Third-Generation: The Advanced Players
This group doesn’t just block beta receptors-they also open up blood vessels. That’s a game-changer.
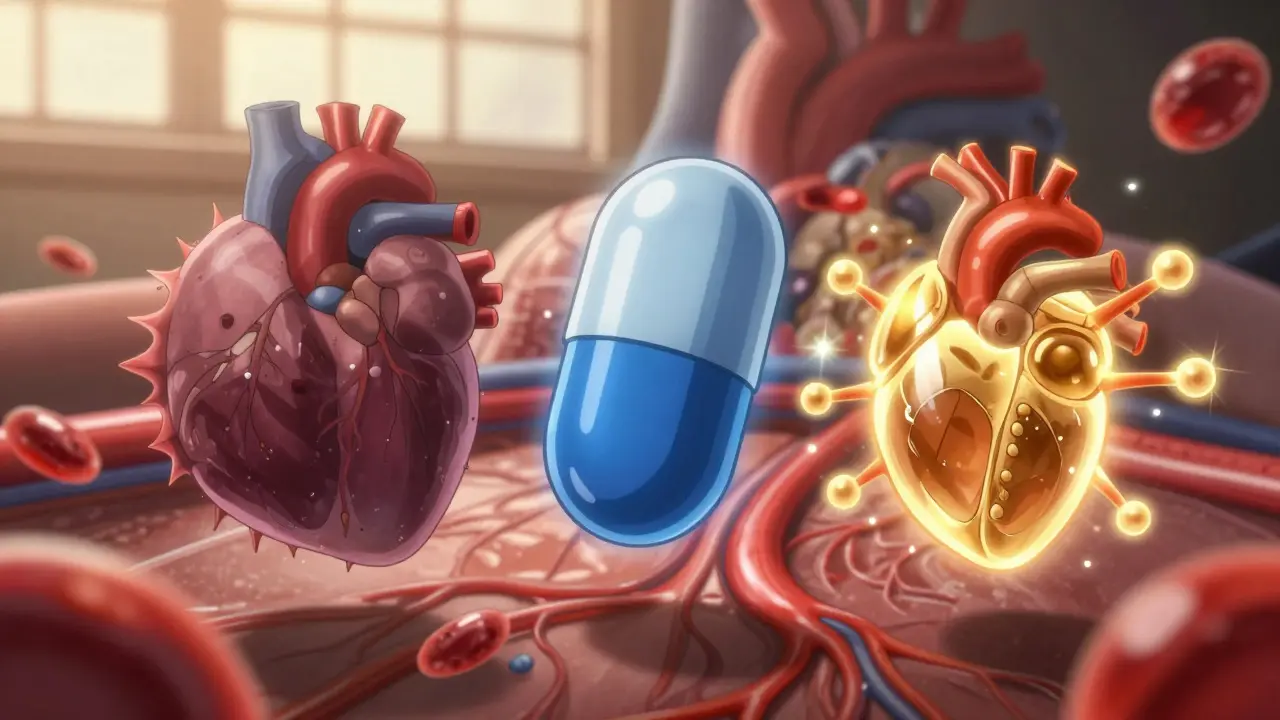
Carvedilol blocks both beta-1 and beta-2 receptors, but it also blocks alpha-1 receptors. That means it dilates arteries, reducing resistance and lowering blood pressure even more. In the US Carvedilol Heart Failure Study (1996), it cut death risk by 35% compared to placebo. It also has strong antioxidant effects, reducing oxidative stress in heart tissue by 30-40% in lab studies. That helps prevent remodeling-when the heart gets bigger and weaker after injury.
Nebivolol (Bystolic) is even more unique. It blocks beta-1 receptors and activates beta-3 receptors, which triggers nitric oxide release. Nitric oxide relaxes blood vessels, improves blood flow, and protects the heart lining. In the SENIORS trial, it lowered cardiovascular death by 14% in elderly heart failure patients. Men over 50 on nebivolol often report better sexual function-65% in one Reddit survey said their libido improved, compared to only 35% on older beta-blockers.
Both carvedilol and nebivolol are now first-choice for heart failure with reduced ejection fraction, according to the European Society of Cardiology. They’re not just symptom controllers-they change the disease’s course.
Why Drug Choice Isn’t One-Size-Fits-All
Here’s where things get real. Your doctor doesn’t just pick a beta-blocker because it’s on a list. They match it to your life.
- If you have asthma or COPD, avoid nonselective blockers like propranolol. Use bisoprolol or nebivolol instead.
- If you have heart failure, carvedilol or nebivolol are preferred. Metoprolol succinate works too, but not tartrate.
- If you’re over 65 and have high blood pressure, avoid atenolol. It doesn’t protect your brain or kidneys as well as others.
- If you’re a man over 50 and worried about sexual side effects, nebivolol is your best bet.
- If you’re on other meds-like antidepressants or diabetes drugs-carvedilol might interact more than bisoprolol.
Even dosing matters. Carvedilol must be started at 3.125 mg twice daily and slowly increased over 8-16 weeks. Rush it, and you risk low blood pressure or fainting. Bisoprolol can be titrated faster-over 4-8 weeks. Metoprolol tartrate needs twice-daily dosing; succinate is once daily. Miss a dose of tartrate? Your heart rate spikes. Miss one of succinate? Not so much.
What Happens If You Stop Suddenly?
Never quit beta-blockers cold turkey. The FDA issued a warning in 2021: stopping abruptly increases your risk of heart attack by 300% in the first 48 hours. Your heart gets flooded with adrenaline it’s been blocked from for weeks. It can trigger dangerous arrhythmias or chest pain.
Always taper down under medical supervision. Even if you feel fine, your body isn’t. The same goes for switching from one beta-blocker to another. You can’t just swap propranolol for carvedilol and expect it to work the same way. Dosing, timing, and effects need careful adjustment.
Real-World Trends and What’s Coming
The beta-blocker market is shifting fast. In 2022, 85% of prescriptions were for second- and third-generation drugs. Propranolol? Only 15% of revenue, even though it’s cheap. Why? Because outcomes matter more than cost.
Heart failure patients are the biggest users-88% get a beta-blocker. But for simple high blood pressure? Only 35% are prescribed one now. Guidelines from Mayo Clinic and ACC/AHA moved them out of first-line because they don’t lower central aortic pressure as well as ACE inhibitors or ARBs.
New developments are on the horizon. In 2023, the FDA approved entricarone-a combo beta-3 agonist and beta-1 blocker-for heart failure with preserved ejection fraction. Early results show 22% fewer hospitalizations. Nebivolol and valsartan combo pills are expected in 2024. And researchers are testing gene-based selection: matching your DNA to the best beta-blocker for you.
But here’s the bottom line: beta-blockers aren’t going away. They’re just getting smarter. For heart failure, post-heart attack, and certain arrhythmias, they’re still the gold standard. The key is choosing the right one-and knowing why.
Can I take a beta-blocker if I have asthma?
Yes, but only if it’s a cardioselective beta-blocker like bisoprolol, metoprolol succinate, or nebivolol. Nonselective ones like propranolol can trigger severe bronchospasm. Even with selective agents, start low and go slow. Always have a rescue inhaler on hand, and avoid high doses. Your doctor should monitor you closely.
Why is carvedilol better than metoprolol for heart failure?
Carvedilol blocks both beta and alpha receptors, which reduces blood vessel resistance and improves blood flow. It also has antioxidant properties that reduce heart tissue damage by 30-40%. In clinical trials, it cut death risk by 35% compared to placebo. Metoprolol succinate works too, but carvedilol has stronger evidence for reversing heart remodeling and lowering long-term mortality.
Do beta-blockers cause weight gain?
Some do, especially older ones like propranolol and atenolol. They can slow metabolism and increase fluid retention. Newer agents like nebivolol and carvedilol are less likely to cause weight gain. If you notice unexplained weight gain-more than 5 pounds in a week-tell your doctor. It could be fluid retention, not fat.
Can beta-blockers affect my sex life?
Yes, some do-especially propranolol and metoprolol tartrate. They can lower libido and cause erectile dysfunction. Nebivolol is different. It boosts nitric oxide, which improves blood flow to the genitals. Studies show 65% of men over 50 on nebivolol reported better sexual function, compared to only 35% on older beta-blockers.
How long does it take for beta-blockers to work?
For heart rate and blood pressure, you’ll notice changes within days. But for heart failure or long-term protection, it takes weeks to months. Carvedilol and nebivolol require slow titration over 8-16 weeks to reach full benefit. Don’t expect immediate results. The goal isn’t just symptom relief-it’s preventing long-term damage.
What to Do Next
If you’re on a beta-blocker, ask your doctor: Which one am I on? Why was it chosen? Is there a better fit for my conditions? Don’t assume all beta-blockers are equal. Your health depends on the right match.
Keep a log: note your heart rate, energy levels, sleep, and side effects. Bring it to your next visit. If you’re on propranolol and feel tired all the time, or on metoprolol tartrate and keep forgetting the second dose-there are better options. The science has moved on. So should your treatment.

Comments
John Rose
Beta-blockers are one of those meds where the devil’s in the details. I used to be on propranolol for anxiety and kept waking up feeling like I’d been run over by a truck. Switched to bisoprolol and suddenly I could climb stairs without gasping. It’s not magic-it’s pharmacology. If your doctor just hands you a script without explaining why, ask for more. You deserve that.
Mark Alan
OMG I JUST GOT OFF METOPROLOL TARTARATE AND MY SEX LIFE IS BACK 🎉🔥 I thought I was doomed to be a zombie with ED forever. Nebivolol? Bro. It’s like my heart and my junk got a VIP pass. America needs to stop prescribing ancient drugs like it’s 1998.
Amber Daugs
People who don’t take their meds exactly as prescribed are why healthcare costs are insane. If you’re going to stop beta-blockers cold turkey because you ‘feel fine,’ you’re not just irresponsible-you’re dangerous. And yes, I’m talking to you, Mr. ‘I’ll just switch to nebivolol myself.’ You don’t get to play doctor.
Ambrose Curtis
Yo, if you got asthma and your doc gave you propranolol, run. Not walk. RUN. I had a cousin who nearly died because they didn’t know the difference between selective and non-selective. Beta-1 vs beta-2 isn’t just jargon-it’s life or death. And yeah, carvedilol’s the real MVP for heart failure. It’s not just about slowing your heart-it’s about healing it. Antioxidant effects? Yeah, that’s not a marketing buzzword, that’s science. Also, if you’re on it, don’t skip doses. The titration? Painful but necessary. Slow wins the race.
And for real-nebivolol for libido? 100% true. My uncle went from ‘I don’t even try anymore’ to ‘honey, let’s go out’ in 6 weeks. Weird side effect? Maybe. Worth it? Hell yes.
Atenolol’s cheap? Sure. But it’s like using a hammer to fix a Rolex. It works, kinda, but you’re gonna break something. Doctors still prescribe it because insurance likes it. Not because it’s best. Question everything.
And if you think weight gain is just ‘eating more’-nah. Propranolol and atenolol mess with your metabolism like a glitchy app. Nebivolol and carvedilol? Not so much. Track your weight weekly. If it jumps 5 lbs in a week, it’s fluid. Tell your doc. Don’t wait.
Gene-based selection? That’s the future. We’re not guessing anymore. We’re mapping. Your DNA doesn’t lie. Imagine a world where your beta-blocker is chosen by your genes, not your doctor’s habit. That’s coming. And honestly? It’s about time.
Robert Cardoso
Let’s be honest: this entire post is a glorified pharmaceutical marketing pamphlet. Beta-blockers are not ‘changing the course of disease’-they’re symptom managers with a side of placebo effect. The 35% mortality reduction? That’s relative risk. Absolute risk reduction is closer to 2%. And the ‘antioxidant effects’? Lab studies on rats, not humans. The real reason carvedilol is pushed? Profit margins. Nebivolol costs 5x more than metoprolol. Who benefits? Not you.
And the ‘sex life improvement’? Correlation isn’t causation. Maybe men on nebivolol are just less depressed because they’re not on propranolol. Or maybe they’re just happier because they stopped taking a drug that made them feel like zombies. Don’t confuse mechanism with outcome.
Also, ‘don’t stop cold turkey’-yes, but why? Because the industry needs you addicted to their $200/month pills. Tapering is standard for any CNS-acting drug. That’s not a feature-it’s a requirement. Stop acting like beta-blockers are holy relics.
Katie Mccreary
I took propranolol for 3 years and lost 20 lbs of muscle. My boyfriend left me because I was ‘emotionally dead.’ Now I’m on nebivolol and I cried during a Disney movie. Who knew?
SRI GUNTORO
In my country, we don’t need fancy pills. We eat turmeric, drink warm water, and pray. Beta-blockers are Western arrogance disguised as science.
Kevin Kennett
For anyone scared to ask their doctor about switching: just say, ‘I’ve been reading up, and I’m wondering if there’s a better option for my asthma/sex life/energy levels.’ Most docs will be thrilled you’re engaged. I used to be terrified to speak up-until I realized my doctor actually wants me to understand. Knowledge is power, and you’re not being annoying-you’re being proactive. You got this.
Howard Esakov
Only a layperson would think beta-blockers are ‘personalized medicine.’ The truth? It’s still shotgun prescribing with a fancy label. Carvedilol? Nebivolol? Just branded versions of the same old mechanism. The real innovation is in the price tag, not the pharmacology. And don’t get me started on the ‘65% improved libido’ claim-sample size? 12 guys on Reddit. That’s science now?
Rhiannon Bosse
EVERYONE KNOWS THE PHARMA COMPANIES CONTROL THE GUIDELINES. CARVEDILOL IS PUSHED BECAUSE IT’S PATENTED. NEBIVOLOL? A $400/MONTH SCAM. THEY’RE ALL THE SAME. THEY JUST REBRANDED PROPRANOLOL AND CALLED IT ‘ADVANCED.’ THE FDA IS A SHAM. I SAW A DOCUMENT LEAKED ON 4CHAN-THEY’RE ALL JUST DIFFERENT COLORS OF THE SAME POISON. 🕵️♀️💀