When you're breastfeeding and need to take medication, it's natural to worry: is this going to hurt my baby? You’re not alone. Millions of new mothers face this exact question every year. The good news? You don’t have to choose between your health and your baby’s safety. With the right timing, you can drastically reduce how much medicine your baby gets through breast milk - sometimes by more than 75%.
Why Timing Matters More Than You Think
Medications don’t just sit in your body. They move. After you swallow a pill, your body absorbs it, sends it into your bloodstream, and eventually, some of it finds its way into your breast milk. But here’s the key: that transfer isn’t constant. It follows a pattern based on your body’s chemistry. Most drugs reach their highest concentration in your blood - and therefore your milk - about 1 to 3 hours after you take them. That’s called the peak plasma concentration. If you breastfeed right after taking your medicine, your baby gets the biggest dose possible. But if you wait until that peak has passed, you cut exposure significantly. The science behind this isn’t new. The Academy of Breastfeeding Medicine (ABM) published detailed guidelines in 2022, building on decades of research. Their Protocol #21 shows that for many common medications, shifting your breastfeeding schedule by just a few hours can drop your baby’s exposure from dangerous levels to safe ones.How Much Medicine Actually Gets to the Baby?
Not all drugs are created equal. The amount your baby receives is measured by something called the Relative Infant Dose (RID). This number compares the dose your baby gets through milk to the dose you took, adjusted for weight. The rule of thumb? If the RID is under 10%, the drug is generally considered safe. But some drugs push close to or above that line. For example:- Codeine: RID 0.6-8.1% - safe for most, but risky for moms who are ultra-rapid metabolizers (a genetic trait that turns codeine into too much morphine too fast).
- Morphine: RID 9.0-35% - high variability. Timing is critical.
- Oxycodone: RID around 10-15% - FDA warns it can cause breathing problems in 1 in 5 exposed infants.
- Tramadol: RID 2.9% - but unpredictable metabolism makes it risky regardless of timing.
- Diazepam: Half-life of 44-48 hours - timing doesn’t help much because it builds up over days.
- Alprazolam: Half-life of 11 hours - much better for timing strategies.
For drugs like morphine or oxycodone, even small changes in timing can mean the difference between a safe exposure and a dangerous one. That’s why timing isn’t just helpful - it’s essential.
Best Practices for Timing Your Medication
Here’s what works in real life, based on guidelines from the ABM, AAP, and CDC:- Take your medicine right after breastfeeding. This gives your body time to clear the drug before the next feeding. For most short-acting drugs, wait 2-3 hours before nursing again.
- Choose immediate-release over extended-release. Extended-release pills (like “XR” or “ER”) release medicine slowly over hours or days. That means your baby gets a steady trickle of the drug - no matter when you nurse. Stick to tablets that act fast and fade fast.
- Use the lowest effective dose. Don’t take more than you need. A lower dose means less goes into your milk.
- Plan ahead for long-acting drugs. If you’re on a medication with a long half-life - like diazepam or fluoxetine - timing won’t help much. Talk to your doctor about alternatives that are safer for breastfeeding.
- Use a pump-and-store strategy if needed. If your baby feeds every 2-3 hours and you’re on a drug with a 4-hour peak, pump and save milk before taking your dose. Then feed your baby the stored milk during the high-exposure window.
For example: If you’re prescribed hydrocodone for pain after delivery, take it right after you nurse at 8 p.m. Then wait until 11 p.m. or midnight before nursing again. That gives your body 3-4 hours to clear most of the drug. Your baby gets far less - and you still get the pain relief you need.
Which Medications Are Safest While Breastfeeding?
Some drugs are so safe that timing barely matters. These are your first-line choices:- Acetaminophen (Tylenol): RID under 2%. Safe anytime.
- Ibuprofen (Advil, Motrin): RID under 1%. Breaks down quickly in milk. Preferred for pain and inflammation.
- Pseudoephedrine (Sudafed): May slightly reduce milk supply, but doesn’t harm the baby. Use short-term.
- Most antibiotics (penicillin, cephalosporins): Low transfer. Rarely cause issues.
For mental health medications, immediate-release SSRIs like sertraline are preferred over long-acting ones. Sertraline has an RID of less than 1%, and its metabolites are inactive in babies. Fluoxetine, on the other hand, has a half-life of up to 7 days - not ideal for timing.
What About Opioids? Can You Still Breastfeed?
Yes - but with caution. The FDA has issued black-box warnings for codeine and tramadol because of unpredictable metabolism. Some mothers process these drugs into morphine too quickly, leading to dangerous levels in breast milk. Even with perfect timing, these drugs are risky. Avoid them if you can. Hydrocodone and morphine are safer options - if timed correctly. The ABM recommends breastfeeding before taking opioids, then waiting 2-3 hours before the next feed. For mothers on buprenorphine for opioid use disorder, the 2022 ABM update recommends dosing right after nursing, with a 3-hour gap before the next feed.What About the First Few Days After Birth?
Don’t panic if you need pain meds right after delivery. In the first 3-4 days, your milk volume is low - often just teaspoons at a time. Even if a drug transfers into colostrum, the total amount your baby receives is tiny. Timing matters less during this phase. Focus on getting rest and healing. You can fine-tune your schedule once your milk supply ramps up.When Timing Doesn’t Help
Some drugs are just not compatible with breastfeeding - no matter when you take them.- Long half-life drugs: Diazepam, fluoxetine, lithium - they stick around for days. Timing won’t clear them fast enough.
- Sustained-release formulations: These are designed to release medicine slowly. That means your baby gets a constant low dose.
- Chemotherapy, radioactive drugs, or recreational substances: These are absolute no-gos. Breastfeeding must stop.
If you’re on one of these, talk to your doctor about alternatives. There’s almost always a safer option.
Who Should You Talk To?
Not all doctors know the details. A 2021 CDC survey found only 35% of general practitioners give specific timing advice. But lactation consultants? 78% do. Make sure you tell everyone who prescribes you medicine: your OB-GYN, your dentist, your pharmacist, your psychiatrist - that you’re breastfeeding. Ask: “Is this safe? What’s the best time to take it?” Use the LactMed database (run by the U.S. National Library of Medicine) to look up any medication. It’s free, updated quarterly, and lists RID values, half-lives, and timing recommendations for over 1,000 drugs.Real-Life Example: Sarah’s Story
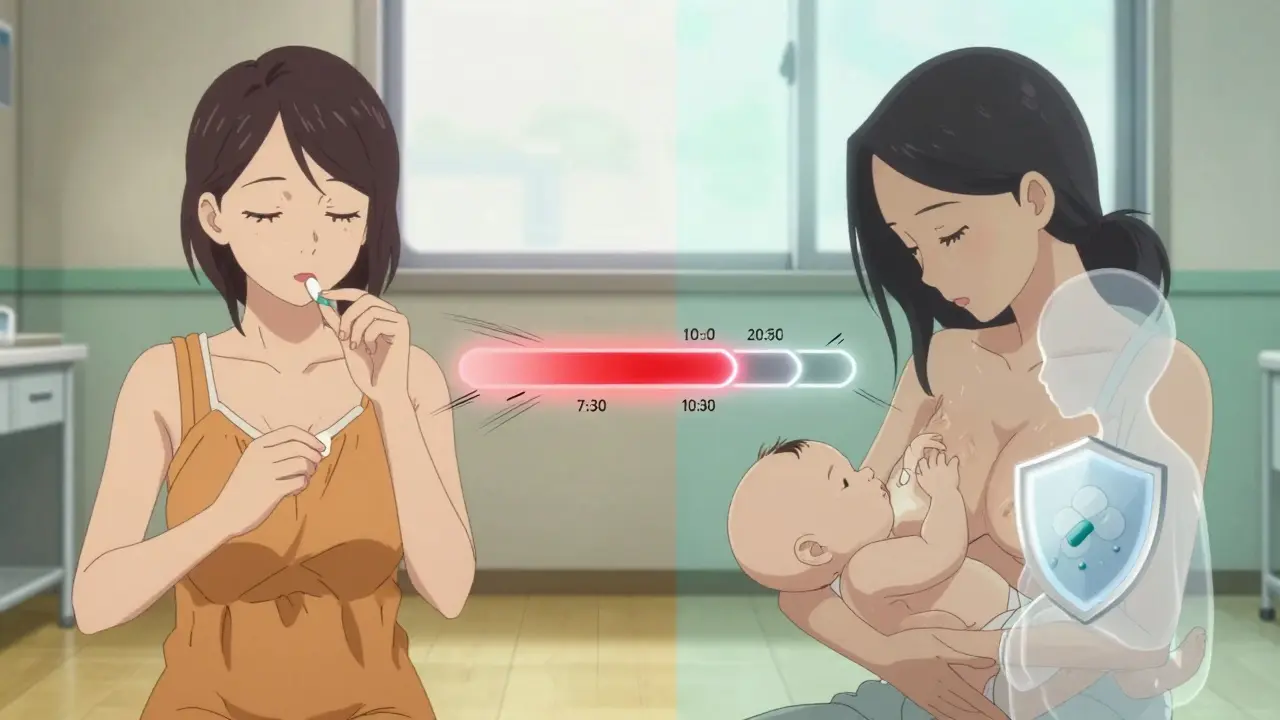
Sarah had a C-section and was prescribed oxycodone. She was terrified. Her pediatrician told her to stop breastfeeding. But her lactation consultant said: “Let’s time it.” They set a schedule:- Feed baby at 7 a.m. → take oxycodone at 7:30 a.m.
- Next feed at 10 a.m. → wait until 10:30 a.m. to nurse.
- Feed at 1 p.m. → take pill at 1:30 p.m.
She pumped and stored milk before her first dose, just in case. After two days, she felt confident. Her baby slept well, fed normally, and showed no signs of drowsiness. She kept breastfeeding for 8 months.
Timing didn’t just protect her baby - it gave her peace of mind.
Final Thoughts: You Don’t Have to Choose
You can take the medicine you need and still breastfeed. The key isn’t avoiding drugs - it’s mastering timing. For short-acting medications, waiting 2-3 hours after your dose before nursing can cut your baby’s exposure in half. For long-acting ones, talk to your doctor about switching to safer alternatives. The goal isn’t perfection. It’s balance. Your health matters. Your baby’s safety matters. And with the right information, you can have both.Can I breastfeed if I take painkillers after delivery?
Yes. Acetaminophen and ibuprofen are safe to take while breastfeeding. For stronger painkillers like oxycodone or hydrocodone, take them right after you nurse, then wait 2-3 hours before the next feeding. Avoid codeine and tramadol - they carry serious risks even with timing.
How long should I wait after taking medicine before breastfeeding?
For most short-acting medications, wait 2-3 hours after taking the dose. This lets your body clear the peak concentration from your blood and milk. For drugs like morphine or hydrocodone, this timing reduces infant exposure by up to 75%. For long-acting drugs like diazepam, timing doesn’t help - talk to your doctor about alternatives.
Is it safe to pump and dump after taking medication?
Pumping and dumping doesn’t speed up how fast the drug leaves your system. It only removes milk that’s already made. If you’re on a short-acting drug, it’s better to time your doses and feed before the peak. Pumping and storing milk before your dose is a better strategy than dumping after.
What if my baby sleeps through the night? Do I still need to time my meds?
Yes. Even if your baby sleeps 6-8 hours, the drug is still in your system. If you take your dose right before bed, you might be feeding during the peak concentration window. To be safe, take your medication right after your last feeding of the day, and wait at least 2-3 hours before the next feed - even if that means waking up to pump.
Can I breastfeed while taking antidepressants?
Many antidepressants are safe. Sertraline and paroxetine have low transfer into milk and are preferred. Avoid fluoxetine and citalopram if possible - they stay in your system longer. Always use the lowest effective dose. Timing helps slightly, but the choice of medication matters more than the schedule.
Where can I find reliable information about my specific medication?
Use LactMed, a free, evidence-based database from the U.S. National Library of Medicine. It lists drug levels in breast milk, infant exposure, and timing recommendations for over 1,000 medications. Talk to a lactation consultant or pharmacist who specializes in breastfeeding - they can help you interpret the data.
Do all medications pass into breast milk?
Almost all medications enter breast milk to some degree - but the amount is usually tiny. What matters is whether that amount is harmful. Many drugs, like acetaminophen and ibuprofen, transfer in such small amounts they’re considered safe. Others, like certain chemotherapy drugs or radioactive compounds, are not. Always check the drug’s safety profile before taking it while breastfeeding.


Comments
siva lingam
So let me get this straight... I take a pill, wait 3 hours, and my baby gets less drug than if I just didn't take it at all? Wow. Science is wild. I'm just glad my kid doesn't need meds beyond Tylenol and crying.
Phil Maxwell
This is actually really helpful. I didn't realize timing mattered this much. I've been taking ibuprofen right before bed and wondering why my baby was so sleepy. Guess I'll start doing it after the last feed. Thanks for laying it out like this.
Shelby Marcel
omg i just realized i’ve been taking my zoloft at 7am and nursing at 8am 😭 i thought i was being good by not skipping feeds. guess i need to switch to sertraline and wait till after i pump. thanks for the wake up call 🙏
Tommy Sandri
The clinical precision of the ABM guidelines presented here is commendable. The distinction between pharmacokinetic profiles of short- and long-acting agents, coupled with the quantification of Relative Infant Dose, represents a significant advancement in evidence-based lactation support. Healthcare providers would benefit from standardized integration of these protocols into routine postpartum care.
Sushrita Chakraborty
I appreciate the thoroughness of this post, but I must emphasize: while timing is critical, it is not a substitute for professional consultation. Every mother's metabolism, every infant's weight and health status, and every medication's pharmacodynamics are unique. Please do not rely solely on online advice-even from reputable sources-without discussing your specific case with a certified lactation consultant or maternal-fetal medicine specialist.
Josh McEvoy
so i took oxycodone after my 2am feed... and then slept till 8am 😅 baby woke up screaming at 8:30... was it the meds?? or just being a toddler? 🤔 anyone else have this happen? 🥲
Heather McCubbin
People are overcomplicating this. If you're on opioids you're already risking your baby's life. Just stop breastfeeding. It's not that hard. Your health doesn't matter more than their lungs. Stop pretending timing makes it okay
Sawyer Vitela
LactMed is the only source you need. Everything else is noise. 80% of this post is redundant. Check the database. Done.
Elizabeth Cannon
Hey new moms-don't stress if you're overwhelmed. I was terrified after my c-section too. I used LactMed, talked to my lactation consultant, and pumped before my first dose. My baby is now 10 months old and thriving. You're doing better than you think. And if you need to switch to formula? That's okay too. Your worth isn't tied to your milk supply. 💪❤️