Opioid Rotation Calculator for Nausea Reduction
Current Opioid Selection
Nausea Reduction Results
Key Considerations:
- Rotation requires 50-75% dose reduction when switching to methadone
- Do not switch without medical supervision
- Most effective when nausea persists beyond 14 days
When you're taking opioids for chronic pain, nausea isn't just an inconvenience-it can make you quit your medication. About one in five people on long-term opioids deal with nausea that doesn't go away, even after weeks or months. This isn't a side effect that fades with time for everyone. For some, it sticks around, making daily life harder and pain harder to manage. The good news? There are real, evidence-backed ways to fight it-through what you eat, how you drink, and which medications actually help.
Why Opioids Make You Nauseous (And Why It Doesn't Go Away)
Opioids don't just block pain signals. They also hit receptors in three key places that trigger nausea: the brainstem's chemoreceptor trigger zone, the inner ear's balance system (vestibular apparatus), and your gut lining. That’s why you might feel queasy even when you haven't eaten, or why turning your head in bed makes it worse. Most people build tolerance within a week or two. But about 15-20% don’t. For them, nausea becomes a chronic problem-no matter how stable the dose.
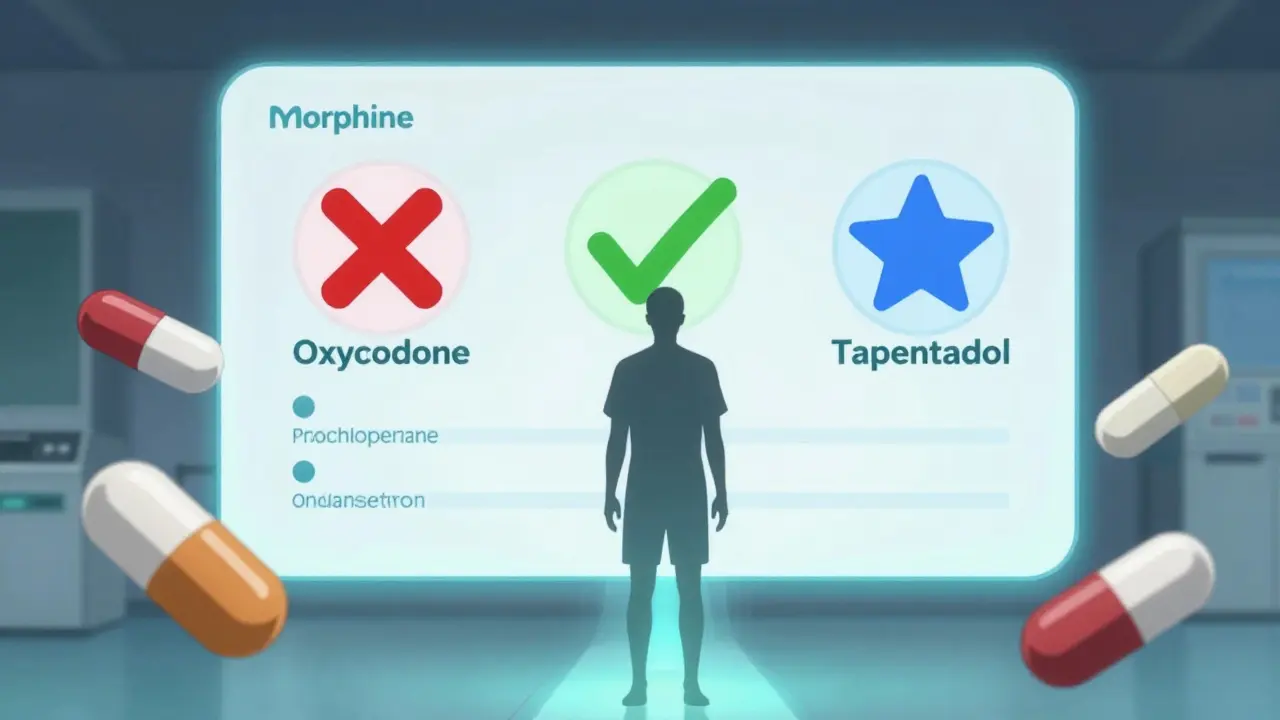
This isn't random. Some opioids are far worse than others. Oxymorphone? High risk. Tapentadol? Much lower. Switching from morphine to oxycodone or a fentanyl patch can cut nausea by half for some people. It’s not a guess-it’s based on receptor binding data and clinical outcomes from over 1,500 patients studied by the European Association for Palliative Care.
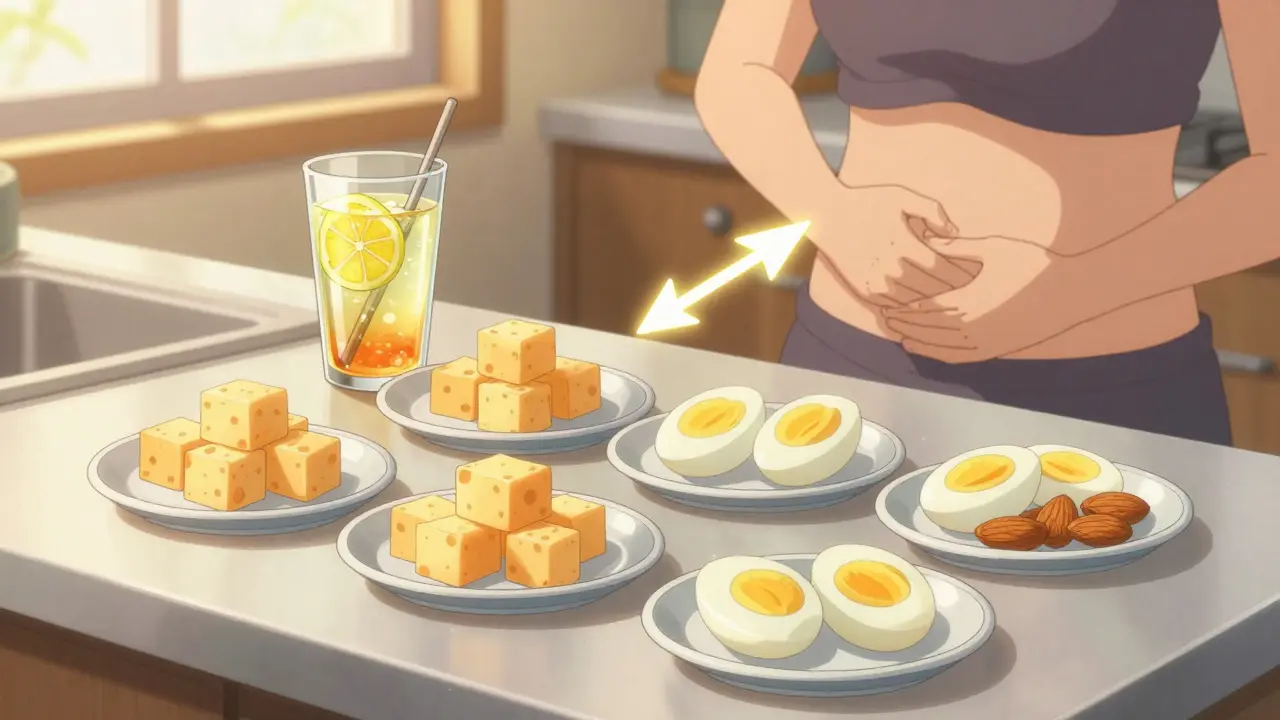
Diet: Small Meals, Protein, and What Actually Helps
You’ve probably heard to eat bland, low-fat foods. But patient surveys tell a different story. In a 2023 survey of 429 chronic pain users, 63% said protein-rich snacks like cheese, nuts, or boiled eggs helped more than crackers or toast. Why? Protein slows stomach emptying just enough to reduce the surge of gastric pressure that triggers nausea. Eating six to eight small meals a day-around 150-200 calories each-cuts nausea in over half of patients, according to a University of Washington pain clinic study.
Ginger is another standout. Not tea. Not supplements. Real ginger chews-like Briess Ginger Chews-showed moderate to significant relief in 78% of 89 users on PainNewsNetwork.org. The active compounds in ginger block serotonin receptors in the gut, the same way some anti-nausea drugs work. Try one chew every 4-6 hours. No need for high doses. Just consistent, real ginger.
Hydration: Sip, Don’t Gulps
Drinking eight glasses of water a day? That advice might backfire. Large volumes stretch the stomach, which can trigger nausea. Instead, sipping 2-4 ounces every 15-20 minutes works better. A 2020 multicenter study found 47% of patients had less severe nausea with this approach.
Electrolytes matter too. Plain water doesn’t always cut it. Patients on Reddit’s r/ChronicPain and PatientsLikeMe consistently report better results with electrolyte drinks like Pedialyte or homemade versions (water + pinch of salt + squeeze of lemon + teaspoon of honey). Opioids can subtly shift fluid balance, and replacing lost sodium and potassium helps stabilize your system. Avoid sugary sodas-they spike blood sugar and worsen stomach upset.
Medication Options: What Works, What Doesn’t
Not all antiemetics are created equal. Here’s what the data says:
- Prochlorperazine (Compazine): First-line for most. 65-70% effective. Cheap. $2-5 per dose. Works by blocking dopamine in the brainstem. Best taken as a tablet or suppository.
- Metoclopramide (Reglan): Only prokinetic available in the U.S. Works by speeding up stomach emptying. About 60% effective. But it carries a black box warning for tardive dyskinesia after 12 weeks. Use only short-term unless closely monitored.
- Promethazine (Phenergan): Similar to prochlorperazine. Sedating. Good for nighttime use. Less effective than prochlorperazine for opioid-induced nausea.
- Ondansetron (Zofran): Blocks serotonin. Great for breakthrough nausea. 60-70% effective. But $35 per dose. Worth it if other options fail.
- Haloperidol: Less effective than phenothiazines. Only 55-60% success. Not recommended as first choice.
- Corticosteroids (dexamethasone): Variable results. 40-50% effective. Mechanism unclear. Sometimes used in cancer patients but not routinely for chronic pain.
One overlooked trick? Head rest. Heuser’s 2017 study showed keeping your head still reduced nausea by 35-40%. No fancy gear needed. Just lie still. Avoid sudden movements. Even propping your head up slightly on pillows at night helps.
Opioid Rotation: The Hidden Game-Changer
If nausea sticks around after 14 days, don’t just add more antiemetics. Consider switching opioids. This is called rotation-and it’s one of the most effective strategies.
Studies show:
- Switching from morphine to oxycodone cuts nausea in nearly half of patients.
- Fentanyl patches often cause less nausea than oral morphine. The steady absorption avoids the spikes that trigger the brainstem.
- Tapentadol has 3-4 times lower nausea risk than oxycodone. It’s not just a painkiller-it’s a gentler option.
But rotation isn’t simple. You can’t just swap one for another. A 50-75% dose reduction is needed when switching to methadone due to incomplete cross-tolerance. Always do this under medical supervision. The goal isn’t to stop pain control-it’s to keep it going without the nausea.
What Doesn’t Work (And Why)
Some common advice falls flat:
- Eye closure: It helps a little-only 5-7% more than head rest alone. Not worth the effort.
- Large, infrequent meals: They overload the stomach. Small, frequent wins every time.
- High-dose ginger supplements: No evidence they’re better than chews. And they can interact with blood thinners.
- Waiting for tolerance: If it’s been over 14 days and you’re still nauseated, tolerance likely won’t come. Don’t wait.
Real-World Challenges
Many patients are stuck in a loop: nausea → fear of nausea → anxiety → worse nausea. About 38% of chronic cases are fueled by this cycle. It’s not just physical-it’s psychological. Simple breathing exercises or mindfulness apps can help break it.
Another problem? Doctors don’t always know. Only 42% of primary care practices have formal protocols for managing opioid-induced nausea. That’s why patients often end up switching meds on their own-sometimes safely, sometimes not. If your doctor doesn’t mention rotation or antiemetics, ask. You have a right to pain relief without constant nausea.
The Future Is Coming
Research is moving fast. A new drug targeting the vestibular system (kappa-opioid receptor blocker) is in Phase III trials and could hit the market by 2025. Low-dose naltrexone (0.5-1 mg daily) is showing 45% reduction in nausea severity in early trials. And gut microbiome studies suggest future treatments might involve prebiotics or probiotics tailored to your unique gut flora.
But for now, the tools we have work-if used right. Diet, hydration, medication choice, and opioid rotation aren’t just options. They’re the core of a practical, evidence-based plan.
How long does opioid-induced nausea last before it becomes chronic?
Opioid-induced nausea becomes chronic if it persists beyond 14 days despite a stable opioid dose. While most people develop tolerance within 3-7 days, about 15-20% of long-term users continue to experience nausea, which is then classified as chronic opioid-induced nausea (OINV).
Can changing my opioid medication help with nausea?
Yes. Switching opioids-called opioid rotation-can significantly reduce nausea. For example, moving from morphine to oxycodone or fentanyl patches has been shown to cut nausea in nearly half of patients. Tapentadol also has 3-4 times lower nausea risk than oxycodone. Always do this under medical supervision with proper dose adjustments.
Is ginger really effective for opioid-induced nausea?
Yes. Real ginger chews (not supplements) have shown moderate to significant relief in 78% of users in one patient survey. Ginger blocks serotonin receptors in the gut, similar to anti-nausea drugs. Try one chew every 4-6 hours. Avoid high-dose supplements-they lack evidence and can interact with medications.
What’s the best antiemetic for opioid-induced nausea?
Prochlorperazine is generally the most effective and affordable first-line option, with 65-70% efficacy. Metoclopramide works well but carries risks with long-term use. Ondansetron is good for breakthrough nausea but expensive. Avoid haloperidol as a first choice-it’s less effective than phenothiazines.
Should I drink more water to reduce opioid nausea?
Drinking large amounts of water can make nausea worse. Instead, sip 2-4 ounces every 15-20 minutes. Electrolyte-enhanced fluids like Pedialyte often work better than plain water because opioids can disrupt fluid balance. Avoid sugary drinks-they spike blood sugar and irritate the stomach.
Can diet alone manage opioid-induced nausea?
Diet alone isn’t enough for most people, but it’s a powerful tool. Eating six to eight small, protein-rich meals daily reduces nausea in 55% of patients. Combine it with sipping fluids, ginger, and-if needed-a low-dose antiemetic. Lifestyle changes work best as part of a broader plan.
Why do some people never develop tolerance to opioid nausea?
Tolerance varies due to genetics, opioid type, and individual receptor sensitivity. People with CYP2D6 poor metabolizer status (like some with codeine) are more prone to persistent nausea. Also, opioids that strongly activate vestibular receptors (like oxymorphone) are harder for the body to adapt to. There’s no test to predict who it’ll affect-so if nausea lasts beyond two weeks, don’t assume it’ll go away.

