Decongestant Safety Checker
Is This Decongestant Safe for You?
Many cold medicines contain decongestants that can dangerously raise blood pressure. This tool helps you determine if a decongestant is safe based on your health conditions.
Safety Assessment
What to do:
- This decongestant is safe for you to use.
- Consider safer alternatives like saline nasal spray or steam inhalation.
- STOP taking this decongestant immediately. Contact your doctor or pharmacist immediately.
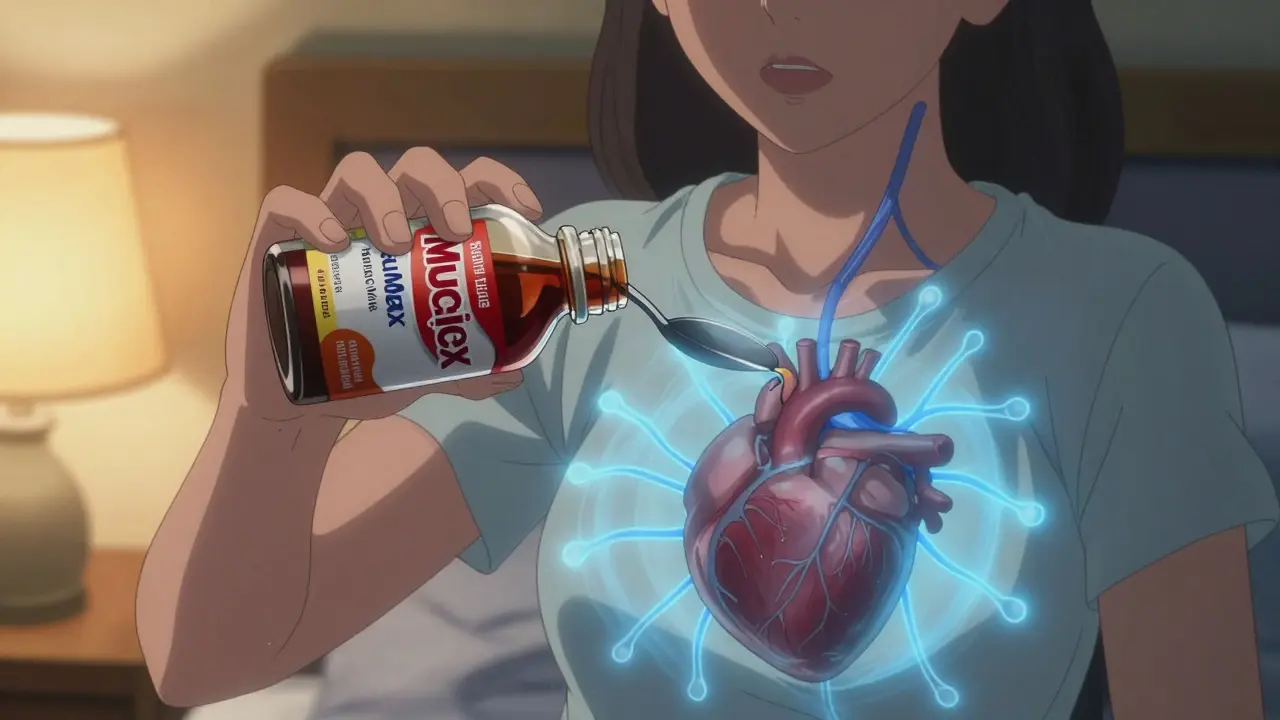
Many people reach for decongestants when they have a cold or sinus infection. It’s quick, easy, and available without a prescription. But if you have high blood pressure, that little bottle of Sudafed or Mucinex Sinus Max could be doing more harm than good. The truth is, decongestants aren’t just harmless nasal sprays-they’re powerful chemicals that can spike your blood pressure, trigger heart palpitations, and even lead to a stroke or heart attack in vulnerable people.
How Decongestants Work (and Why They’re Dangerous for Hypertension)
Decongestants like pseudoephedrine and phenylephrine work by narrowing blood vessels in your nose. That reduces swelling and mucus, helping you breathe. But here’s the catch: they don’t stop at your nasal passages. These drugs tighten blood vessels all over your body, including in your heart and kidneys. That increases resistance in your circulatory system, forcing your heart to pump harder. The result? A rise in blood pressure.
It’s not just a small bump. Studies show that pseudoephedrine can raise systolic blood pressure by 5 to 10 mm Hg on average. For someone with controlled hypertension, that might seem minor. But for someone with uncontrolled blood pressure, heart disease, or a history of arrhythmias, it’s enough to push them into danger. A 2023 meta-analysis in US Pharmacist confirmed that even at standard doses, pseudoephedrine causes measurable increases in blood pressure-especially with immediate-release forms.
Which Decongestants Are the Riskiest?
Not all decongestants are the same. The most common and well-studied is pseudoephedrine, found in Sudafed and many multi-symptom cold remedies. It’s been linked to heart attacks, strokes, and dangerous heart rhythms in people with high blood pressure. Because of this, it’s sold behind the pharmacy counter in the U.S. and requires a pharmacist to screen for contraindications.
Phenylephrine, now the most common decongestant in OTC products since pseudoephedrine was restricted, was once thought to be safer. But recent research tells a different story. A 2023 case study in US Pharmacist documented a 5-year-old child who developed high blood pressure after taking a phenylephrine-based cold syrup. Her pressure returned to normal only after stopping the medication. This suggests phenylephrine isn’t any safer than pseudoephedrine-it just hasn’t been studied as long.
Other decongestants to avoid include:
- Ephedrine (rarely used now but still in some supplements)
- Naphazoline (found in some nasal sprays)
- Oxymetazoline (Afrin, Dristan, and others)
Even nasal sprays like Afrin can be risky if used for more than 3 days. They cause rebound congestion and can be absorbed into the bloodstream, leading to systemic effects.
What Happens When Decongestants Meet Blood Pressure Meds?
It’s not just the decongestant itself that’s dangerous-it’s what it does when mixed with your regular blood pressure medication. Beta-blockers, ACE inhibitors, diuretics, and calcium channel blockers all work to lower blood pressure. But decongestants fight against them. The result? Your meds become less effective. Your blood pressure creeps up, and you might not even notice.
One 2023 report from the American Heart Association found that nearly 1 in 5 hypertensive patients using decongestants saw their blood pressure rise enough to require an emergency visit. Many didn’t realize their cold medicine contained a decongestant because it was buried in a multi-symptom formula.
Here are common products that contain hidden decongestants:
- Tylenol Cold and Flu
- Advil Multi-Symptom Cold and Flu
- Benadryl Allergy Plus Congestion
- Mucinex Sinus Max
- Theraflu Cold & Flu
- Robitussin CF
Always read the active ingredients list-not just the brand name. Look for these words: pseudoephedrine, phenylephrine, ephedrine, oxymetazoline.
Who Is at Highest Risk?
Not everyone with high blood pressure will have a bad reaction. But some people are far more vulnerable:
- Those with uncontrolled hypertension (BP over 140/90)
- People with heart disease, including prior heart attacks or heart failure
- Patients with irregular heart rhythms (like atrial fibrillation)
- Those with Prinzmetal angina (a rare type of chest pain caused by artery spasms)
- Anyone taking MAO inhibitors (antidepressants like Nardil or Parnate)
- Older adults on multiple medications
Even if your blood pressure is under control, your heart may still be under stress. Decongestants can trigger arrhythmias or sudden spikes in pressure that you won’t feel until it’s too late.
What Should You Do Instead?
You don’t have to suffer through congestion. There are safer ways to clear your nose without risking your heart:
- Saline nasal spray or rinse (like a neti pot)-no drugs, no side effects
- Steam inhalation-breathe in warm, moist air from a bowl of hot water
- Humidifiers-especially at night-help keep nasal passages moist
- Antihistamines without decongestants-like loratadine (Claritin) or cetirizine (Zyrtec)-if allergies are the cause
- Hydration and rest-your body heals better when you’re not dehydrated or exhausted
These alternatives won’t work as fast as a decongestant, but they’re far safer. And for many people, they work just as well over time.

What to Do If You’ve Already Taken a Decongestant
If you have high blood pressure and accidentally took a decongestant:
- Stop taking it immediately
- Check your blood pressure if you have a home monitor
- Watch for symptoms: headache, dizziness, chest pain, rapid heartbeat, blurred vision
- If your BP is over 180/110 or you feel unwell, seek medical help
- Call your doctor-even if you feel fine. A spike might not cause symptoms right away
Pharmacists are trained to catch these mistakes. When you buy pseudoephedrine, they ask about your health because they know the risks. Don’t be embarrassed to say you have high blood pressure. That’s exactly why the questions exist.
The Bigger Picture: Why This Keeps Happening
It’s not just about ignorance. The problem is built into how OTC meds are sold. Companies package decongestants into multi-symptom formulas because they sell better. Consumers assume "cold medicine" means "safe for everyone." But it’s not. The American Society of Health-System Pharmacists estimates that 15% of hypertensive patients still use decongestants despite warnings.
Even more troubling? Many elderly patients are on five or more medications. A single cold medicine can add a hidden drug that interacts with their heart pills, kidney meds, or diabetes drugs. The risk grows with age.
The American Heart Association launched a "Medication Check-Up" campaign in 2022 to address this. Their message is simple: "Just because it’s over-the-counter doesn’t mean it’s safe for you."
Final Advice: Protect Your Heart
If you have high blood pressure:
- Never assume an OTC medicine is safe
- Always read the active ingredients list
- Ask your pharmacist: "Does this contain a decongestant?"
- Keep a list of your medications and share it with every doctor
- Use saline sprays and steam as your first line of defense
- Monitor your blood pressure more often during cold season
Decongestants aren’t evil. But they’re not harmless either. For someone with high blood pressure, they’re a hidden trigger. The best way to stay healthy isn’t to avoid colds-it’s to choose safe ways to treat them.

