Understanding Uremic Bleeding and Its Challenges
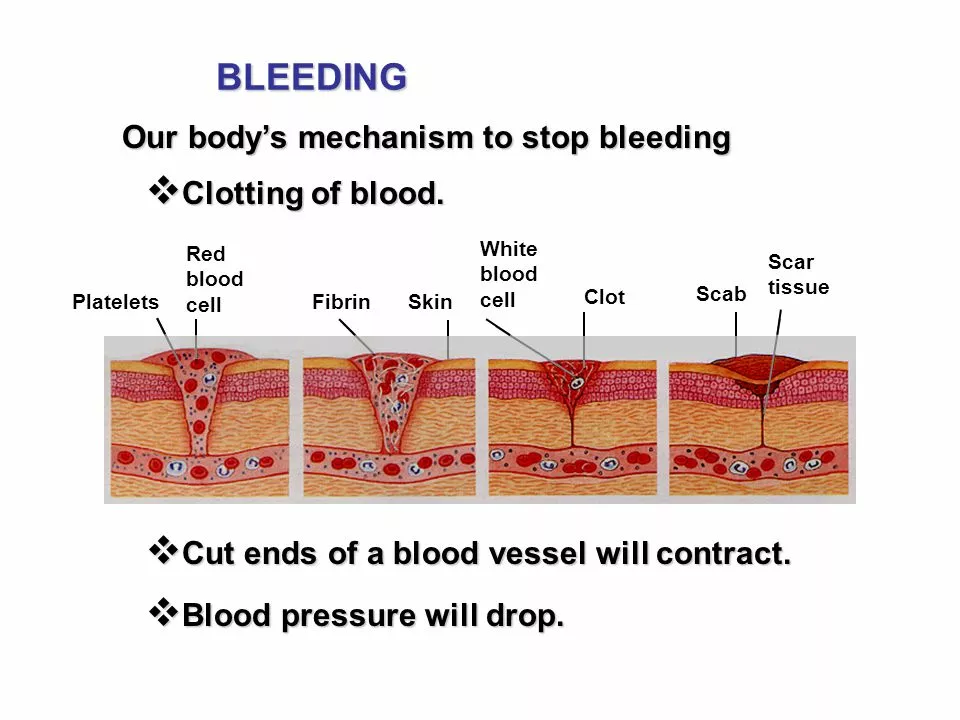
Uremic bleeding is a common complication experienced by patients with chronic kidney disease, especially those undergoing dialysis. This condition is characterized by an increased tendency towards bleeding due to abnormalities in the blood clotting process. This can lead to a variety of symptoms, ranging from spontaneous bruising and prolonged bleeding after minor injuries to more severe life-threatening bleeding events.
As a patient, it's essential to understand the challenges uremic bleeding presents in the management of chronic kidney disease. In this section, we will discuss the underlying causes of uremic bleeding, its impact on the patient's quality of life, and the need for more effective treatment options to minimize the risks associated with this condition.
An Overview of Desmopressin as a Treatment Option
Desmopressin is a synthetic analog of the antidiuretic hormone vasopressin, which has been used in the treatment of various bleeding disorders for several decades. Its primary mechanism of action is to stimulate the release of von Willebrand factor (vWF) from endothelial cells, which plays a crucial role in blood clotting.
Due to its ability to improve platelet function and reduce bleeding time, desmopressin has been considered a potential treatment option for uremic bleeding. In this section, we will provide a comprehensive overview of desmopressin, its pharmacological properties, and its potential benefits in the management of uremic bleeding.
Reviewing Clinical Studies on Desmopressin in Uremic Bleeding
Over the years, several clinical studies have investigated the efficacy and safety of desmopressin in the treatment of uremic bleeding. These studies have shown mixed results, with some demonstrating a significant reduction in bleeding time and others reporting no significant improvement.
In this section, we will review the most relevant clinical studies on desmopressin in uremic bleeding, highlighting the key findings, limitations, and potential implications for clinical practice. This will provide a better understanding of the current evidence base supporting the use of desmopressin in this patient population.
Addressing Concerns about Desmopressin Side Effects
As with any medication, the use of desmopressin in the treatment of uremic bleeding is not without potential side effects. Some of the most common side effects reported with desmopressin use include headache, facial flushing, and mild abdominal pain. More serious side effects, such as hyponatremia and thrombotic events, have also been reported in rare cases.
In this section, we will address the concerns about desmopressin's side effects and discuss strategies to minimize the risks associated with its use. This will help patients and healthcare providers make informed decisions about incorporating desmopressin into their treatment plans.
Comparing Desmopressin to Other Treatment Options
While desmopressin has shown promise as a potential treatment for uremic bleeding, it's essential to consider its benefits and risks in the context of other available treatment options. These options may include blood transfusions, erythropoietin-stimulating agents, and the use of antifibrinolytic agents, such as tranexamic acid.
In this section, we will compare desmopressin to other treatment options for uremic bleeding and discuss the potential advantages and disadvantages of each approach. This information will help patients and healthcare providers make more informed decisions about the most appropriate treatment strategy for their individual needs.
Future Directions for Desmopressin Research and Development
Despite the mixed results from clinical studies on desmopressin in uremic bleeding, there is still much to learn about its potential role in the management of this condition. Ongoing research is needed to better understand the factors that may influence the response to desmopressin treatment and to identify patient subgroups that may benefit the most from this therapy.
In this section, we will discuss the future directions for desmopressin research and development, including potential new indications, novel formulations, and strategies to optimize its use in the treatment of uremic bleeding. This will provide a glimpse into the future of desmopressin therapy and its potential impact on the lives of patients with chronic kidney disease.

Comments
Beth Lyon
Ive had a few dialysis sessions where the bruising just wouldn’t stop and thinking about desmopressin seemed like a glimmer of hope even though the info out there is kinda scattered.
Nondumiso Sotsaka
It’s great that you’re digging into the research 🙌 keep exploring the options and remember that every patient’s response can be different 😊
Ashley Allen
Desmopressin can help some uremic patients with bleeding.
Brufsky Oxford
When we contemplate the balance between clotting and bleeding, desmopressin stands as a modest philosopher in the hematologic arena :) it nudges vWF release, reminding us that even tiny hormonal whispers can shift the tide of haemostasis.
Lisa Friedman
Actually the pharmacodynamics of DDAVP are well‑documented; it triggers endothelial release of vWF and factor VIII, improving platelet adhesion. Clinical trials from the 90s showed reductions in bleeding time by up to 30%, though later studies were less conclusive. Keep in mind the hyponatremia risk, especially in dialysis patients with limited fluid excretion – that’s a key safety concern.
cris wasala
Don’t let the mixed data scare you we all learn from each case and build better protocols together keep the optimism alive and watch the outcomes
Tyler Johnson
Desmopressin’s role in uremic bleeding is a nuanced topic that deserves a thorough, step‑by‑step walk through. First, we recognize that uremic platelets suffer from impaired aggregation, largely due to reduced vWF multimers and altered glycoprotein IIb/IIIa function. Second, DDAVP can temporarily counteract this by stimulating endothelial cells to release vWF, thereby enhancing platelet‑vessel wall interaction. Third, the timing of administration matters; giving the drug shortly before a planned invasive procedure often yields the best hemostatic benefit. Fourth, dosage must be individualized – a standard 0.3 µg/kg IV bolus is common, but some clinicians prefer a slower infusion to mitigate the risk of hyponatremia. Fifth, monitoring serum sodium after DDAVP is essential, especially in patients with limited renal clearance, because water retention can precipitate dangerously low sodium levels. Sixth, not all patients respond; a bedside bleeding time test or platelet function assay can help identify responders versus non‑responders. Seventh, adjunctive therapies such as tranexamic acid may synergize with DDAVP, offering a multimodal approach to bleeding control. Eighth, the literature reports both positive outcomes – reduced bleeding episodes and transfusion requirements – and neutral or negative findings, underscoring the heterogeneity of study designs and patient populations. Ninth, side‑effects beyond hyponatremia, like mild headaches or flushing, are usually self‑limited, but clinicians should stay vigilant for rare thrombotic events. Tenth, cost considerations matter; DDAVP is relatively inexpensive compared to some newer agents, making it accessible in resource‑limited settings. Eleventh, patient education is crucial – informing them about fluid intake restrictions after dosing can prevent complications. Twelfth, future research should aim to stratify which sub‑groups – perhaps those with residual platelet function – gain the most benefit. Thirteenth, integrating DDAVP into standardized bleeding protocols can streamline care pathways and reduce variability. Fourteenth, interdisciplinary collaboration between nephrologists, hematologists, and surgeons ensures the drug is used judiciously. Finally, the decision to employ desmopressin should balance potential hemostatic gains against the individual’s risk profile, always keeping patient safety at the forefront.
Annie Thompson
Reading all the data feels like wading through a stormy sea of numbers and anecdotes the way the heart aches when you see bruises you cant explain is something we all feel deeply and yet the promise of a single drug feels almost like a whisper of hope in that dark night but we must not forget the shadows of side effects that linger like unwanted guests at a party sometimes the hyponatremia comes in quietly and you only notice the dizziness later the balance is fragile and each patient’s story adds another layer to the tapestry of our understanding.
Parth Gohil
From a pathophysiological standpoint, uremic toxins impair platelet‑glycoprotein interactions, and DDAVP’s action via V2‑receptor agonism restores some of the missing vWF multimers – a classic example of targeted pharmacology addressing a mechanistic deficit. Moreover, we should consider the pharmacokinetic nuances in dialysis patients where drug clearance differs markedly from non‑renal cohorts.
VAISHAKH Chandran
One must question whether this so‑called miracle drug truly merits the fanfare or merely serves as a convenient scapegoat for our therapeutic inadequacies the elite discourse often glosses over the low‑grade evidence while painting a picture of revolutionary change
Pat Merrill
Oh wow, another “potential breakthrough” – because we definitely needed more hype in the literature, right? Honestly, the data is as solid as a wet paper towel, but hey, at least it gives us something to talk about at conference coffee breaks.
Vicki Roth
I wonder how the dosing intervals intersect with the timing of dialysis sessions – that’s something worth keeping an eye on for optimal effect.
Vishal Bhosale
Not convinced the benefits outweigh the hassle simple and clear no big deal
Garima Gauttam
Maybe we’re overthinking it; perhaps the drug works but we’re too busy debating to see the simple truth.
Georgia Nightingale
The drama surrounding desmopressin is almost theatrical – the headlines scream “miracle cure” while the actual studies whisper indecision. As a self‑proclaimed know‑it‑all, I can tell you that the evidence is a mixed bag, and the real story lies in the patient‑specific nuances that get lost in sensationalist summaries.
Chris Kivel
Great overview, keep sharing insights and let’s keep supporting each other in navigating these complex treatment choices
sonia sodano
Honestly, I think the whole focus on desmopressin is a distraction from more promising therapies that deserve our attention.