When you pick up a prescription at the pharmacy and see a generic version of your brand-name drug, you’re seeing the result of one of the most impactful laws in modern U.S. healthcare. The FDA’s authorization of generic drugs isn’t just a shortcut-it’s a carefully designed legal and scientific process that saves patients billions every year. But how exactly does the FDA approve these lower-cost versions? And what’s the real legal foundation behind them?
The Hatch-Waxman Act: The Legal Backbone of Generic Drugs
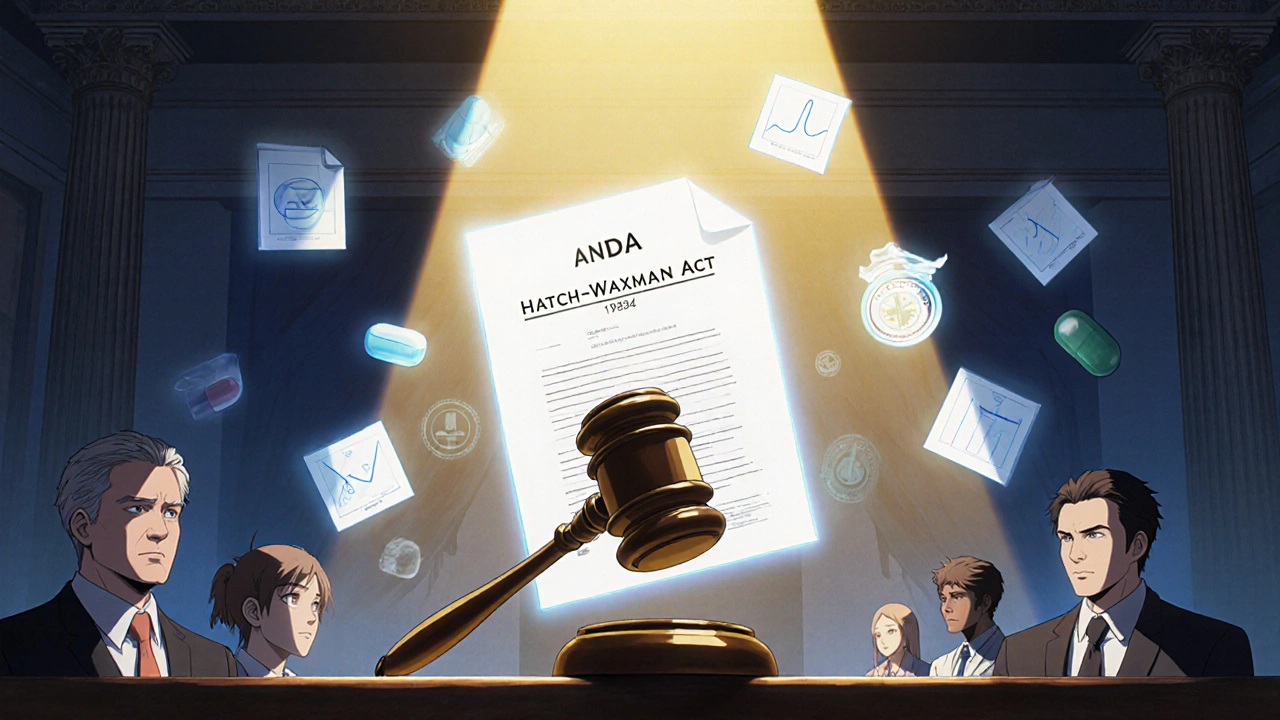
The entire system of generic drug approval in the U.S. traces back to one law: the Drug Price Competition and Patent Term Restoration Act of 1984, better known as the Hatch-Waxman Act. Passed on September 24, 1984, this law didn’t just tweak regulations-it rebuilt the entire framework for how drugs reach the market. Before Hatch-Waxman, generic manufacturers had to repeat every single clinical trial that the original drug maker did. That meant spending hundreds of millions and waiting years just to prove a drug worked. It wasn’t practical. The law changed that by creating the Abbreviated New Drug Application (ANDA) pathway under Section 505(j) of the Federal Food, Drug, and Cosmetic Act. The genius of the ANDA was simple: if a generic drug has the same active ingredient, strength, dosage form, and route of administration as the brand-name drug-and if it’s shown to work the same way in the body-then you don’t need to retest safety and effectiveness from scratch. The FDA already did that. The generic maker just needs to prove they can replicate it. This wasn’t just about cost. It was about access. Today, 9 out of every 10 prescriptions filled in the U.S. are for generic drugs. That’s not an accident. It’s the direct outcome of this law.What the FDA Actually Requires for Approval
The FDA doesn’t approve generics lightly. There’s no "good enough" in drug regulation. Every approved generic must meet the exact same standards as the brand-name version. Here’s what that means in practice:- Same active ingredient: The chemical that makes the drug work must be identical. No exceptions.
- Same strength and dosage form: If the brand is a 20mg tablet, the generic must be a 20mg tablet-not a capsule, not a liquid, not a 15mg version.
- Same route of administration: If the original is taken orally, the generic must be taken orally. If it’s injected, the generic must be injected the same way.
- Same use indications: The generic can’t be approved for fewer or different conditions than the brand.
- Bioequivalence: This is the key. The generic must deliver the same amount of active ingredient into the bloodstream at the same rate as the brand. The FDA requires this to be proven through studies in 24-36 healthy volunteers, measuring blood levels over time.
- Identical quality standards: The generic must meet the same batch requirements for identity, strength, purity, and stability. No corners cut.
- Same manufacturing standards: The facility making the generic must follow the same Good Manufacturing Practices (GMP) as the brand-name maker. The FDA inspects these sites-sometimes unannounced.
The ANDA Submission: What’s in the File
Submitting an ANDA isn’t just filling out a form. It’s a massive scientific and regulatory package. Here’s what’s required:- Chemistry, Manufacturing, and Controls (CMC): Detailed documentation on how the drug is made, including raw materials, equipment, and quality control tests.
- Facility information: All manufacturing, packaging, and testing sites must be listed and inspected.
- Proposed labeling: The drug’s package insert must match the brand’s in content and format.
- Bioequivalence data: Full study reports, including statistical analysis, from human trials.
- Patent certifications: The applicant must certify whether the brand’s patents are expired, invalid, or will be infringed. A Paragraph IV certification-challenging a patent-can trigger legal battles and delay approval.
Review Timelines and GDUFA
The timeline for approval has changed dramatically since 1984. Back then, the law said the FDA had 180 days to review an ANDA. But as applications piled up, delays stretched to years. The solution came with the Generic Drug User Fee Amendments (GDUFA), first enacted in 2012 and renewed in 2022 as GDUFA III. This program lets the FDA collect fees from generic manufacturers to fund more reviewers and faster processing. Today, the FDA’s goal is:- 10 months for a standard original ANDA
- 8 months for priority applications-like first generics or drugs in short supply
Why Some Generics Take Longer-And Why They’re Harder
Not all generics are created equal. Simple pills? Easy. Complex drugs? Not so much. The ANDA pathway was designed for small-molecule drugs-like metformin, lisinopril, or atorvastatin. These are chemically straightforward. But what about inhalers, topical creams, or extended-release tablets? These are considered "complex generics." For these, bioequivalence isn’t enough. The FDA needs more data. How does the drug behave in the lungs? How does it release over time in the stomach? How does it absorb through the skin? These questions require specialized testing-sometimes animal studies, sometimes advanced imaging. The FDA has a dedicated initiative called "Complex Generic Drug Product Development Resources" to help manufacturers navigate these challenges. But it’s still harder, slower, and more expensive. That’s why there are fewer complex generics on the market-and why prices stay higher.
Patents and Market Exclusivity: The Hidden Delays
Even if a generic is ready to go, it might not hit the market right away. Why? Patents. The Hatch-Waxman Act lets brand-name companies list their patents in the FDA’s "Orange Book." When a generic applicant files a Paragraph IV certification-claiming a patent is invalid or won’t be infringed-the brand can sue. And if they do, the FDA can’t approve the generic for up to 30 months. This is called the "30-month stay." It’s a legal tool, not a scientific one. It’s often used to delay competition. In some cases, brands file multiple patents on minor changes-like a new coating or packaging-to extend protection. This is called "patent thickets." The FDA’s Drug Competition Action Plan tries to counter this by identifying drugs with little competition and pushing for faster generic entry. But it’s an ongoing battle.Who Makes These Generics? And How Big Is the Market?
The U.S. generic drug market was worth about $125 billion in 2022. That’s a huge chunk of the $450 billion total pharmaceutical market. And it’s growing. Major players include Teva, Sandoz, Viatris (which merged Mylan and Upjohn), and Amneal. But there are hundreds of smaller companies too, especially those focusing on niche or complex generics. The real winners? Patients. Generic drugs cost, on average, 80-85% less than their brand-name equivalents. That’s not a small saving. It’s life-changing for people on fixed incomes, chronic conditions, or without good insurance. Take naltrexone extended-release injectable suspension, approved as a generic in 2023. The brand version, Vivitrol, was used to treat opioid addiction. The generic made it affordable for more people in recovery. The FDA called it "of prime importance"-and rightly so.What’s Next? The Future of Generic Approval
The FDA isn’t resting. In October 2025, they launched a new pilot program to speed up ANDA reviews for companies that test and manufacture their drugs in the U.S. The goal? Strengthen the domestic supply chain and reduce reliance on overseas production. There’s also growing focus on biosimilars-generic versions of biologic drugs like insulin or cancer treatments. But those follow a different legal path under the Biologics Price Competition and Innovation Act (BPCIA), not the Hatch-Waxman Act. For traditional generics, the system works. It’s not perfect. There are delays, complex products, and patent games. But the core framework-rigorous science, clear rules, and a focus on patient access-has delivered results. The FDA’s mission is simple: get safe, effective, affordable drugs to the public as quickly as possible. And for generics, they’ve done exactly that.Are generic drugs as safe as brand-name drugs?
Yes. The FDA requires that generic drugs meet the same strict standards for safety, strength, quality, and performance as brand-name drugs. They use the same active ingredients and are held to identical manufacturing rules. Millions of people take generics every day without issue.
Why do generic drugs look different from brand-name drugs?
By law, generics can’t look exactly like the brand-name version-that would violate trademark rules. So they may have different colors, shapes, or inactive ingredients like fillers or dyes. But the active ingredient, dosage, and effect are identical.
How long does it take for a generic to be approved after a brand drug’s patent expires?
It depends. If no one challenges the patent, the first generic can be approved within 10 months of submitting a complete ANDA. But if a brand company sues over patent infringement, the FDA can be blocked for up to 30 months. Some generics face delays of years due to legal battles.
Can a generic drug be pulled from the market after approval?
Yes. If the FDA finds quality issues, manufacturing violations, or safety concerns after approval, they can recall the product. This has happened with several generics in recent years due to contamination or failed stability tests. The FDA monitors approved generics just like brand drugs.
Are all generic drugs made in the U.S.?
No. Most active pharmaceutical ingredients (APIs) are made overseas, especially in India and China. But the FDA inspects all manufacturing sites-whether in the U.S., India, or elsewhere-to ensure they meet U.S. standards. The new pilot program aims to encourage more U.S.-based production.

Comments
Brad Seymour
Love how this breaks down the Hatch-Waxman Act without turning it into a law textbook. I’ve been on generic metformin for years and never thought twice about it-until I saw the price difference. My insurance pays $4, the brand costs $200. No brainer. The FDA’s got this right.
Malia Blom
Let’s be real-this whole system is a corporate shell game. The FDA ‘approves’ generics but ignores the fact that 80% of APIs come from India and China, where inspections are performative at best. And don’t get me started on those ‘Paragraph IV’ patent trolls who delay generics for years just to keep prices high. This isn’t healthcare-it’s profit theater.
And yet somehow, we’re supposed to trust that a pill made in a factory with no English labels is ‘bioequivalent’? Yeah right. The science is a smokescreen for global supply chain exploitation.
Erika Puhan
It’s fascinating how the ANDA pathway is framed as a triumph of efficiency, yet the underlying structural inequities are never addressed. The bioequivalence studies rely on homogenous cohorts of healthy volunteers-often college students paid $50 to swallow pills-while the actual patient populations (elderly, comorbid, polypharmacy) are excluded from validation. This is pharmacoeconomic performative science.
And let’s not romanticize cost savings when the downstream burden falls on Medicaid patients who still face prior authorizations and tiered formularies. The FDA approves the drug, but the market doesn’t deliver access. That’s not progress-it’s regulatory optics.
Edward Weaver
China and India making our meds? Are you kidding me? We let foreign countries control the supply chain for life-saving drugs and then act surprised when there’s a shortage? This isn’t ‘affordable healthcare’-it’s national security failure. The FDA’s ‘inspections’ are jokes. I bet half those factories don’t even have running water. We need to bring manufacturing back to the U.S. or we’re one pandemic away from mass death.
And don’t even get me started on ‘complex generics.’ If we can’t make a simple pill right here, what does that say about our tech base? We used to build everything. Now we just take pills made by people who don’t speak English.
Lexi Brinkley
GENERIC DRUGS ARE A MIRACLE 😍 I take 5 of them a day and my bank account still has money 💸 My insulin generic cost $12 vs $400 😭 FDA YOU ARE THE BEST 🙌👏👏👏
Kelsey Veg
u ever notice how generic labels always have weird filler names like 'corn starch' or 'titanium dioxide' but the brand ones say 'proprietary coating'? like... yeah you're using the same junk, you just hid it behind a fancy word. also why do all generics taste like chalk? 🤢
Alex Harrison
Just want to say I’ve been on generic lisinopril for 8 years and never had an issue. The FDA’s standards are actually really solid. I know people get paranoid about foreign manufacturing but if the facility gets inspected and passes, it passes. I don’t need to know who made it, just that it works. And it does. Every time.
Also the 30-month stay thing is ridiculous. Companies abuse that to delay competition. The FDA should have more power to fast-track when patents are clearly flimsy. But overall, this system works better than most people realize.
Jay Wallace
It’s ironic-while we laud the Hatch-Waxman Act as a beacon of innovation, we ignore its fundamental flaw: it was designed for a 1984 pharmaceutical landscape, not a 2025 globalized, algorithm-driven, patent-abuse ecosystem. The ANDA pathway is a relic masquerading as progress.
And yet, we’re told to celebrate the 90 generics approved in 2023… as if quantity equals equity. Where are the real metrics? Patient outcomes? Adverse event reporting disparities? Formulary discrimination? No. We get shiny stats and feel-good headlines.
Meanwhile, the FDA’s new pilot program? A PR stunt. Manufacturing in the U.S.? Sure-unless it’s cheaper to outsource to a facility in Tamil Nadu that pays $2/hour and has zero environmental oversight. The system is rigged. The FDA is a gatekeeper, not a guardian.
And don’t get me started on biosimilars-those are the real frontier. But we’re still stuck arguing about whether a pill made in Bangalore is ‘bioequivalent’ to one made in Ohio… while the real issue is that nobody’s holding Big Pharma accountable for evergreening patents with trivial modifications.
So yes, generics save money. But they don’t save justice. And that’s the real failure.