When you pick up a prescription, you might not think twice about whether it’s a generic or brand-name drug. But behind that choice is a complex system of insurance rules, cost controls, and medical exceptions that can save you hundreds-or cost you thousands. In Australia, the Pharmaceutical Benefits Scheme (PBS) handles this differently than in the U.S., but the core tension remains: generics are cheaper, but are they always the right choice for you?
How Insurance Decides What to Cover
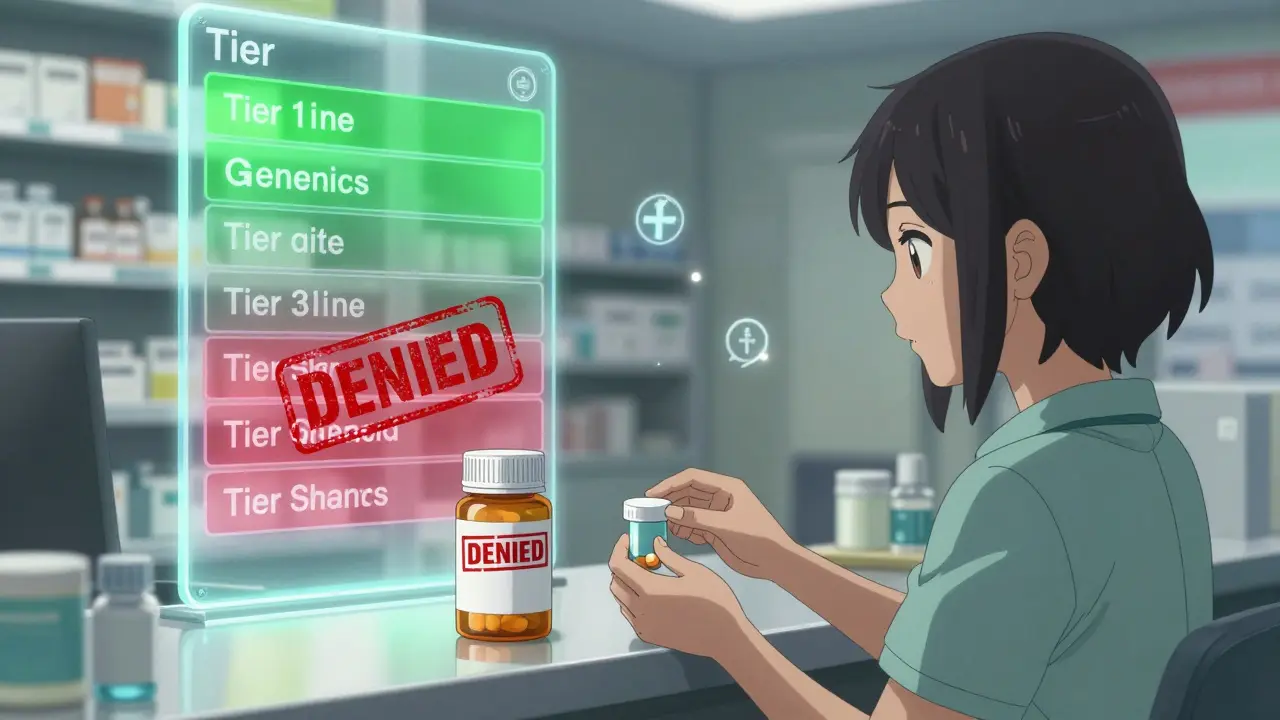
Insurance plans don’t just randomly pick which drugs to cover. They use something called a formulary-a list of approved medications grouped into tiers based on cost and clinical preference. Think of it like a pricing ladder.Generic drugs almost always sit on Tier 1: the lowest copay, often $5 to $15 for a 30-day supply. Brand-name drugs? They’re usually on Tier 2 or 3, with copays jumping to $40, $60, or even higher. Some plans don’t even cover brand-name drugs unless there’s no generic alternative.
Here’s how it works in practice: if your doctor prescribes Lipitor (brand-name atorvastatin), and a generic version exists, your pharmacy will automatically give you the generic unless your doctor writes “dispense as written” on the prescription. That’s not a suggestion-it’s a rule. In fact, 90% of all prescriptions filled in the U.S. are generics, and that number is rising. Why? Because insurers push hard for them. They save billions.
The Cost Difference Isn’t Close
The price gap between generics and brands is massive. A 30-day supply of the brand-name drug Crestor (rosuvastatin) might cost $150 out-of-pocket. The generic? Around $4. That’s a 97% drop. Same active ingredient. Same dosage. Same effect. But the brand-name version carries the cost of research, marketing, and patent protection. Generics skip all that.Insurance companies use this gap to their advantage. Many plans make you pay the difference if you choose the brand. So if the generic costs $5 and the brand costs $100, you pay $5 (the generic copay) plus $95 (the price difference). That’s $100 total. Most people just take the generic.
But here’s the catch: not all generics are created equal. While the active ingredient must match, the fillers, dyes, and binders can vary. For most people, this doesn’t matter. But for those on narrow therapeutic index (NTI) drugs-like warfarin, levothyroxine, or phenytoin-those tiny differences can cause real problems. That’s why 27 U.S. states have special rules allowing brand-name coverage for these drugs without extra paperwork.
When You Can Get the Brand Name Anyway
You might think generics are always the default. But there are legal and medical ways to get the brand name-even when a generic exists.First, your doctor can write “do not substitute” on the prescription. That’s it. No explanation needed in most states. But insurers still push back. They’ll often require you to try the generic first. That’s called step therapy. For 35% of specialty drugs, you have to fail one or two generics before they’ll approve the brand.
Second, you can appeal. If you’ve had side effects, or your condition worsened after switching, you can file a prior authorization request. The average time to get approval? About 3.2 business days. But 41% of those requests need a second call from the doctor. That’s a delay. And if you’re on a medication that needs steady levels-like epilepsy or thyroid drugs-that delay can be dangerous.
Medicare Part D patients have it even tougher. They’re required to use generics unless a doctor proves medical necessity. And even then, the documentation has to follow strict codes. One common code is YN1, used to signal that a brand-name drug is needed despite a generic being available. If you miss the code? Your claim gets denied.
What the Data Really Says
The FDA says generics are just as safe and effective as brand-name drugs. And for most people, that’s true. But data from JAMA Neurology shows a 12.3% higher seizure rate in patients switched from brand to generic antiepileptic drugs. Other studies report patients on generic versions of Wellbutrin XL, Concerta, or Lamictal experiencing reduced effectiveness or new side effects-even though the active ingredient is identical.Why? Because the inactive ingredients can affect how the drug is absorbed. For someone with a sensitive stomach, a different dye might cause nausea. For someone with thyroid disease, a slight variation in absorption could throw off their hormone levels.
Doctors aren’t blind to this. A 2022 survey found that 68% of physicians have seen patients report different side effects with generics. That doesn’t mean generics are bad. It means they’re not one-size-fits-all.
How Patients Get Stuck
Many people don’t realize their insurance changed its formulary. One month, your brand-name drug is covered. The next, it’s not. You refill your prescription, get charged $120, and realize your plan now only covers the generic. You didn’t get a notice. You didn’t know. You just paid more.A Kaiser Family Foundation survey found that 34% of commercially insured patients were confused about when generics were covered. Nearly 20% skipped filling prescriptions because they didn’t want to pay the surprise cost.
On forums like Reddit and Drugs.com, there are thousands of stories from people who switched to a generic and felt worse. One user wrote: “I was stable on brand-name Lamictal for 8 years. Switched to generic. Had my first seizure in a decade. Took 6 months to get the brand back.”
These aren’t rare cases. They’re systemic. And they’re why some states, like California, now require insurers to cover brand-name drugs if a patient has a documented adverse reaction to the generic.

What You Can Do
If you’re on a chronic medication, don’t assume the generic is always the best option. Here’s what to do:- Check your plan’s formulary every year during open enrollment. Things change.
- Ask your pharmacist: “Is there a generic? If so, can I get the brand if needed?”
- If you feel different after switching-fatigue, mood changes, worse symptoms-tell your doctor immediately. Don’t wait.
- Ask your doctor to write “do not substitute” if you’ve had issues before. Keep a copy of that prescription.
- If your claim is denied, file an appeal. Most plans have a 30-day window. Use the medical necessity form. Include your history.
- For Medicare users: Use the Medicare Plan Finder tool. It shows which drugs are covered and at what tier.
And if you’re on a brand-name drug with a high copay, ask your doctor about manufacturer copay cards. Many big pharma companies offer them to reduce out-of-pocket costs to $0-$10. But here’s the catch: Medicare and Medicaid patients can’t use them. It’s illegal. So if you’re on Medicare, you’re stuck with the plan’s rules.
The Bigger Picture
The push for generics isn’t just about saving money. It’s about systemic efficiency. Over the past decade, generics saved the U.S. healthcare system over $2.2 trillion. That’s real money. That’s more people getting care.But the system isn’t perfect. It treats all patients the same. It assumes biology is predictable. It doesn’t account for individual variation. And when it fails, people suffer.
As new drugs-especially complex ones like inhalers, injectables, and biosimilars-enter the market, the rules are changing. Insurers are starting to treat “complex generics” differently. They know these aren’t just pills with different fillers. They’re harder to copy. And they need different rules.
The future of drug coverage won’t be just generic vs. brand. It’ll be smart coverage: matching the right drug to the right patient, based on history, response, and biology-not just cost.
Until then, know your plan. Know your options. And don’t be afraid to ask for what you need.
Can I be forced to take a generic drug?
Yes, in most cases. Insurance plans and pharmacies are required to substitute generics unless your doctor writes “do not substitute” on the prescription. All 50 U.S. states allow this, but some require additional documentation from the prescriber. If you’ve had bad reactions to generics before, ask your doctor to document it and write the prescription accordingly.
Why are generics so much cheaper?
Generics don’t have to repeat expensive clinical trials. They only need to prove they’re bioequivalent to the brand-name drug-meaning they work the same way in the body. That saves manufacturers millions in research and development costs. They also don’t spend money on advertising. Those savings get passed to insurers and patients.
Are generics less effective than brand-name drugs?
For most people, no. The FDA requires generics to have the same active ingredient, strength, dosage form, and route of administration as the brand. But for a small group-especially those on narrow therapeutic index drugs like thyroid meds or seizure medications-differences in inactive ingredients can affect absorption. Some patients report side effects or reduced effectiveness after switching. If you notice changes, tell your doctor right away.
What if my insurance denies my brand-name drug?
You can appeal. Most insurance plans have a formal process. You’ll need documentation from your doctor showing why the generic didn’t work-side effects, worsening symptoms, or therapeutic failure. Some plans require you to try two or three generics first. The process can take days or weeks. If you’re in urgent need, ask your doctor to request an expedited review.
Can I use a manufacturer’s copay card for a brand-name drug?
Yes-if you have commercial insurance. Many drugmakers offer copay cards that reduce your out-of-pocket cost to $0-$10. But if you’re on Medicare, Medicaid, or a government program, you can’t use these cards. It’s against federal law. So if you’re on Medicare, your only option is to appeal for coverage or pay full price.

Comments
John Tran
so like... i just got switched from brand-name Lamictal to some generic crap last month and now i’m having these weird brain zaps like my neurons are doing the cha-cha? i thought generics were supposed to be the same? turns out nope. my neurologist just shrugged and said "it’s bioequivalent" like that’s some kind of magic spell. bioequivalent my ass. i’m not a lab rat. i’m a person who used to sleep through the night and now i’m wide awake at 3am wondering if my soul is leaking out of my ears. also, why does the pill look like a tiny radioactive mushroom? someone please tell me this isn’t normal.
Priyanka Kumari
Thank you for sharing this. It’s so important to recognize that while generics are a vital part of affordable healthcare, they’re not one-size-fits-all. I’ve seen patients in my community struggle silently after switching - fatigue, mood shifts, even seizures in rare cases. The system needs to listen more and assume less. If a patient reports a change, we should treat it as real, not anecdotal. Doctors, pharmacists, and insurers all need to collaborate better. Your story helps make that case.
Avneet Singh
It’s fascinating how the regulatory framework prioritizes cost-efficiency over pharmacokinetic individuality. The FDA’s bioequivalence threshold of 80–125% AUC is statistically permissible but clinically reckless for NTI drugs. The pharmacodynamic variance in excipients - particularly in sustained-release formulations - introduces non-linear absorption profiles that are neither accounted for nor monitored post-market. This is not pharmaceutical equivalence; it’s commoditized substitution masked as therapeutic parity.
Pankaj Singh
Stop crying about generics. If you can’t afford your meds, don’t be a baby. Everyone else takes the generic and lives fine. Your "brain zaps" are probably anxiety. You’re just mad because you got a $5 pill instead of a $150 one. Big Pharma doesn’t care about you - they want you addicted to their overpriced crap. Take the generic, shut up, and be grateful you’re not in India where people pay $0.50 for the same thing.
Robin Williams
bro. i was on brand-name Concerta for 10 years. switched to generic. felt like my brain was wrapped in wet cardboard. tried to explain it to my doc. he said "it’s the same molecule." yeah, but my soul isn’t a molecule. it’s a vibe. and the vibe changed. now i’m back on brand with a copay card. also, why do all generics taste like chalk? is it the fillers? or is it the corporate soul crushing my spirit? 🤔
Kimberly Mitchell
People who complain about generics are either misinformed or exploiting loopholes to profit from overpriced pharmaceuticals. The FDA has stringent standards. If you’re experiencing side effects, it’s likely non-adherence, psychological suggestion, or an undiagnosed comorbidity. Stop blaming the system and start taking responsibility. Your insurance isn’t your therapist. And no, you don’t get to demand brand-name drugs because you "feel different." That’s not medicine - that’s entitlement dressed in medical jargon.
Rosalee Vanness
I want to gently say: if you’ve been stable on a brand-name drug for years and suddenly feel off after switching - don’t ignore it. Don’t let anyone tell you it’s "all in your head." I’ve been there. I switched from brand to generic levothyroxine and went from feeling energized to exhausted, depressed, and foggy for six months. My endocrinologist finally listened after I brought lab results and a symptom journal. We switched back. My TSH normalized within weeks. You are not being dramatic. You are being observant. Document everything. Bring data. Ask for a prior auth. You have a right to be treated as an individual, not a line item.
Trevor Davis
Hey, I just wanted to say I really appreciate this post. I’m a nurse and I see this every day. Patients cry in the pharmacy line because their copay went from $5 to $120 overnight. No notice. No warning. And when they go back to their doctor, the doctor says "oh, I didn’t know they changed the formulary." It’s broken. We need better communication. We need transparency. And we need to stop treating people like numbers on a spreadsheet. I’m not mad - I’m just tired. And I think a lot of us are.
mike swinchoski
Anyone who takes generics is a dumbass. Brand-name drugs are for real people. Generics are for peasants who can’t afford to be healthy. My cousin’s dog gets brand-name heartworm meds. Why? Because it’s not about cost - it’s about quality. You wouldn’t feed your kid store-brand Tylenol, so why take store-brand seizure meds? This system is rigged to make you sick so they can sell you more drugs later. Wake up.
Angel Tiestos lopez
yo i just came back from india and let me tell u - their generic system is wild. $0.20 for the same pill i pay $5 for here. but here’s the twist: they don’t have insurance. so everyone just pays cash. no tiered formularies, no prior auth, no drama. just medicine. and guess what? people are fine. maybe the problem isn’t generics… it’s the middlemen. the insurers. the pharmacies. the bureaucracy. we turned healthcare into a game of monopoly. and we’re all losing.
Acacia Hendrix
The entire debate is a red herring. The real issue is the lack of pharmacovigilance in post-market generic surveillance. Without mandatory real-world outcome tracking for NTI drugs, we’re operating on 1980s-era assumptions. The FDA’s bioequivalence criteria are insufficient for complex formulations. This isn’t about patient preference - it’s about regulatory obsolescence. Until we implement pharmacogenomic-guided substitution protocols, we’re just gambling with lives.
James Castner
Let me offer a systems-level perspective: The $2.2 trillion saved by generics over the past decade has enabled millions of Americans to access life-sustaining medications they otherwise could not afford. This is a monumental public health achievement. That said, systemic inflexibility - particularly the lack of automated, real-time formulary alerts and patient-specific exception workflows - creates preventable harm. The solution is not to abandon generics, but to engineer a dynamic, patient-centered formulary engine that integrates clinical history, pharmacogenomic data, and prior response patterns. We must move from cost-based substitution to outcome-based prescribing. This is not idealism - it is the logical evolution of precision medicine.
Adam Rivera
Just wanted to say - if you’re struggling with a switch, you’re not alone. I had the same thing with my thyroid med. Took me 4 months and 3 doctors to get my brand back. But I kept pushing. I wrote letters. I saved my lab results. I showed up to appointments with printouts. And guess what? They listened. You’ve got a voice. Use it. Don’t let the system make you feel like a burden. You’re not. You’re a human being who deserves to feel like yourself again.
Damario Brown
lol so you took a $4 pill and now you’re having "brain zaps"? maybe you’re just stressed. maybe you’re depressed. maybe you’re just addicted to the idea that you’re special. everyone else takes the generic and doesn’t whine. you’re not sick. you’re entitled. and if you think your body is too "sensitive" for generics, go live in a cave. the world doesn’t care about your vibes.