Diabetes GI Symptom Checker
Assess Your Risk
Answer these questions to determine if your symptoms might be related to diabetes-related gastrointestinal issues.
Your Risk Assessment
Quick Takeaways
- High blood sugar can damage nerves that control the stomach, leading to delayed emptying (gastroparesis).
- Diabetes often alters the gut microbiome, which can aggravate IBS‑like symptoms.
- Frequent nausea, bloating, constipation, or heartburn should prompt a check‑up, especially if blood glucose is poorly controlled.
- Managing blood glucose, eating smaller meals, and targeted medications can dramatically improve digestive comfort.
- Regular screening for autonomic neuropathy helps catch gut issues early.
When you hear the words Diabetes is a chronic metabolic condition characterized by elevated blood glucose due to insufficient insulin production or insulin resistance, you probably think about blood sugar checks, insulin pens, and foot care. What many people miss is that the digestive tract is wired directly into the same nervous and hormonal networks that regulate glucose. In fact, up to 75% of people with long‑standing diabetes report at least one gastrointestinal (GI) symptom. This article untangles why the gut gets pulled into the diabetes story, what problems to watch for, and concrete steps you can take right now.
Why the Gut Gets Involved
Two main pathways link diabetes to digestive trouble:
- Neuropathy - persistent hyperglycemia damages the autonomic nerves that tell the stomach and intestines when to contract, relax, and move food along.
- Metabolic & microbiome shifts - high glucose and insulin fluctuations change the composition of gut bacteria, which in turn affect inflammation, motility, and even hormone release.
Both mechanisms can happen together, creating a feedback loop: poor gut function makes blood sugar harder to control, and erratic sugar levels further impair gut nerves.
Key Gastrointestinal Conditions Linked to Diabetes
Below are the most common GI issues that surface in people with diabetes, along with why they appear.
| Condition | Typical Symptoms | Primary Diabetes‑Related Cause | First‑Line Management |
|---|---|---|---|
| Gastroparesis is delayed stomach emptying caused by autonomic neuropathy | Nausea, early satiety, bloating, erratic blood glucose spikes after meals | Damage to vagus nerve | Low‑fat, low‑fiber meals; pro‑kinetic meds (e.g., metoclopramide); tight glucose control |
| Irritable Bowel Syndrome (IBS) is a functional bowel disorder marked by altered motility and heightened pain perception | Cramping, alternating diarrhea/constipation, gas | Microbiome imbalance + visceral hypersensitivity | Low‑FODMAP diet; probiotics; stress management; regular glucose monitoring |
| Gastro‑esophageal Reflux Disease (GERD) is acid reflux caused by weakened lower esophageal sphincter | Heartburn, sour taste, nighttime cough | Delayed gastric emptying + high‑fat meals | Elevate head of bed; avoid late‑night meals; PPIs if needed; improve glycemic control |
| Constipation is infrequent, hard stools often from slowed colonic transit | Straining, abdominal discomfort, feeling of incomplete evacuation | Autonomic neuropathy + low fluid intake | Increase fiber gradually, hydrate, occasional osmotic laxatives |
How Diabetes‑Induced Neuropathy Disrupts Digestion
Autonomic nerves act like a traffic controller for the gut. In a healthy system, the vagus nerve signals the stomach to contract after you eat, pushes chyme into the small intestine, and then cues the colon to move waste out. When high glucose repeatedly overwhelms blood vessels, the nerves lose their ability to fire accurately-this is diabetic neuropathy is a type of nerve damage caused by chronic hyperglycemia. The result is a sluggish stomach (gastroparesis) or an uneven colon rhythm (constipation).
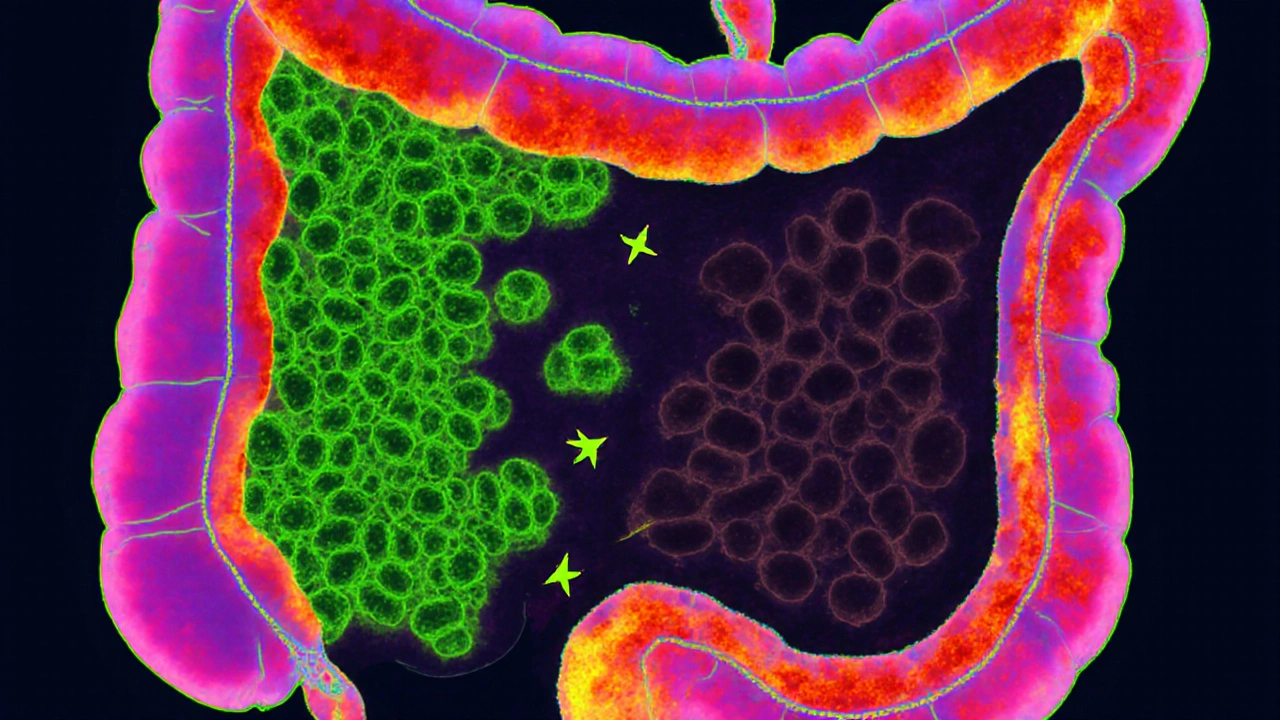
The Role of the Gut Microbiome
Studies from 2023‑2024 show that people with type 2 diabetes have a lower proportion of short‑chain‑fatty‑acid‑producing bacteria such as Faecalibacterium prausnitzii. These microbes normally keep the gut lining tight and reduce inflammation. When they drop, patients often experience bloating, abdominal pain, and erratic bowel movements-classic IBS‑like complaints. Moreover, an altered microbiome can influence how the body metabolizes carbs, feeding the cycle of high blood glucose is the concentration of glucose circulating in the bloodstream after meals.
Spotting the Signs Early
Because symptoms overlap with everyday digestive annoyances, the key is to watch for patterns linked to glucose spikes or drops. Ask yourself:
- Do I feel full after just a few bites, even when I haven’t eaten much?
- Does my blood sugar swing dramatically after a big dinner?
- Am I waking up with heartburn or nausea more often than before?
- Has my stool frequency changed without a clear dietary reason?
If you answer “yes” to several, bring it up at your next endocrinology or primary‑care visit. A simple gastric emptying study or a stool analysis can confirm the diagnosis.

Managing Diabetes‑Related GI Problems
Effective treatment blends three pillars: tighter glucose control, targeted gut‑focused strategies, and lifestyle tweaks.
1. Blood Sugar Tightening
Even modest reductions in HbA1c (0.5‑1%) can slow nerve damage progression. Consider:
- Switching to a basal‑bolus insulin regimen if you’re on oral agents only.
- Trying a GLP‑1 receptor agonist; these drugs slow gastric emptying, which can be a double‑edged sword but often balances post‑prandial spikes.
- Using continuous glucose monitoring (CGM) to spot trends linked to meals that trigger GI flare‑ups.
2. Dietary Adjustments
Many patients find relief by fine‑tuning what they put on the plate:
- Smaller, frequent meals: 4‑6 mini‑meals reduce the workload on a lagging stomach.
- Low‑fat, low‑fiber for gastroparesis: Fat and bulky fiber delay emptying; choose lean proteins, well‑cooked veggies, and refined grains temporarily.
- Low‑FODMAP trial for IBS symptoms: Cut back on onions, garlic, wheat, and certain fruits for 2‑4 weeks, then re‑introduce gradually.
- Hydration: Aim for 2L of water daily unless fluid restriction is medically required.
3. Medications Specific to the Gut
When diet isn’t enough, doctors can prescribe:
- Pro‑kinetics (e.g., metoclopramide, erythromycin) to boost stomach muscle activity.
- Antispasmodics (e.g., dicyclomine) for IBS‑type cramping.
- Acid‑suppressors (PPIs or H2 blockers) for GERD.
- Probiotics containing strains like Lactobacillus rhamnosus that have shown modest improvement in bloating for diabetics.
4. Lifestyle and Stress Management
Stress amplifies both blood sugar and gut pain. Incorporate:
- Mindful breathing or short meditation (10min) before meals.
- Light aerobic activity-walking after dinner helps move food through the GI tract.
- Regular sleep schedule; poor sleep spikes cortisol, worsening both glucose and gut motility.
Prevention: Keeping Your Gut Healthy Before Problems Appear
Think of your gut as a partner in diabetes management. The earlier you protect it, the smoother life gets.
- Screen annually for autonomic neuropathy using heart‑rate variability tests or a simple post‑prandial blood pressure check.
- Maintain a balanced microbiome by eating a variety of plant‑based foods, limiting processed sugars, and considering a daily prebiotic supplement (e.g., inulin).
- Avoid smoking and excessive alcohol, both of which irritate the digestive lining and worsen neuropathy.
- Stay current with vaccinations (e.g., flu, pneumococcal) to prevent infections that can destabilize glucose and gut health.
When to Seek Professional Help
If you notice any of the following, book an appointment promptly:
- Persistent vomiting or inability to keep food down for more than 48hours.
- Sudden, unexplained weight loss.
- Severe, constant abdominal pain not relieved by OTC meds.
- Blood glucose readings that stay high despite medication adjustments.
These signs could indicate advanced gastroparesis, an ulcer, or another serious condition that needs imaging or endoscopy.
Frequently Asked Questions
Can type 1 diabetes cause the same gut problems as type 2?
Yes. Both types expose nerves to chronic high glucose, so autonomic neuropathy and gastroparesis can occur in type 1 as well. However, type 2 often co‑exists with obesity‑related gut inflammation, which can add extra IBS‑like symptoms.
Is a low‑carb diet good for diabetic gut issues?
Lowering carbs helps stabilize blood glucose, which in turn reduces nerve stress. But cut carbs too aggressively and you may lose beneficial fiber that feeds good bacteria. Aim for a moderate low‑carb approach (45‑50g per day) paired with soluble fiber sources like oat bran.
Can probiotics replace medication for diabetic IBS?
Probiotics can lower bloating and improve stool consistency, but they rarely eliminate pain on their own. They work best as an adjunct to diet changes and, if needed, antispasmodic meds.
How often should I be screened for gastroparesis?
If you have symptoms, a simple gastric emptying breath test can be ordered right away. For asymptomatic patients with >10years of diabetes, an annual symptom questionnaire is advised, and testing is recommended if the score rises.
Does exercise help my gut if I have diabetes?
Yes. Moderate aerobic activity (30min, 5days a week) stimulates intestinal motility, improves insulin sensitivity, and reduces stress-all three factors that protect against constipation and gastroparesis.


Comments
Karen Ballard
Great summary! 😊
Gina Lola
Really dive‑deep into the gut‑brain axis, the article nails the mechanistic jargon-autonomic neuropathy, dysbiosis, and gastric emptying latency are all laid out like a protocol. The bit about short‑chain‑fatty‑acid‑producing bacteria is especially on point for anyone tracking microbiome biomarkers. Plus the practical tip on low‑FODMAP trials feels like a real‑world hack rather than just theory. I appreciate the mention of CGM integration for symptom correlation; that kind of data‑driven approach is what clinics need. Overall, it’s a solid blend of pathophysiology and actionable advice.
Leah Hawthorne
The breakdown of gastroparesis versus IBS really helped me sort out what’s hitting my stomach after meals. I’ve been noticing that my blood sugar spikes right after a heavy dinner, and the article’s suggestion to try smaller, low‑fat meals makes sense. Also, the tip about using a pro‑kinetic like metoclopramide if diet alone isn’t enough is something I’ll bring up with my doc. Thanks for the clear, balanced info – it’s not overly clinical but still solid.
Brian Mavigliano
One could argue that the gut is merely a passive conduit for the whims of glycemic chaos, yet the article lifts it to a protagonist in the diabetic saga. First, it paints neuropathy not as a static endpoint but as a dynamic erosion of the vagal highways that orchestrate peristalsis, thereby turning the stomach into a stalled freight depot. Second, the microbiome is introduced not as a decorative side‑character but as a microbial orchestra whose discordant notes amplify inflammation and motility disorders. Third, the feedback loop described – hyperglycemia damaging nerves, nerves failing to regulate glucose, and dysbiosis exacerbating both – is a classic example of a pathological ouroboros. The author wisely suggests that breaking this loop requires a three‑pronged strategy: tighter glucose control, dietary modulation, and targeted pharmacotherapy. In practice, the recommendation to employ low‑FODMAP trials mirrors the precision medicine trend, acknowledging that one‑size‑fits‑all diets are relics of a bygone era. Moreover, the inclusion of continuous glucose monitoring as a diagnostic adjunct underscores the rising importance of data‑driven decision‑making. What truly stands out is the emphasis on regular autonomic neuropathy screening – a preventive measure often sidelined in routine visits. By flagging early signs such as post‑prandial hypotension or heart‑rate variability shifts, clinicians can intervene before full‑blown gastroparesis sets in. Finally, the piece does not shy away from the psychosocial dimension: stress management and sleep hygiene are woven into the therapeutic tapestry, reminding us that the gut‑brain axis is as much about hormones as it is about microbes. In sum, the article presents a comprehensive, systems‑level view that transcends the narrow focus on blood sugar, inviting readers to consider the gut as an active participant in diabetic health.
Emily Torbert
I totally get how overwhelming all this can feel, especially when you’re already juggling insulin doses and daily life. The tip about drinking more water and aiming for 2 L a day is simple but often missed, and it really helps with constipation. Also, don’t underestimate the power of a short walk after meals – it can kick the stomach into gear. If you’re dealing with bloating, a probiotic with Lactobacillus rhamnosus might calm things down a bit. Hang in there, you’re not alone in this.
Rashi Shetty
While the article presents a thorough overview, it inadvertently glosses over the ethical implications of prescribing pro‑kinetic agents without thorough screening. The recommendation to use metoclopramide requires caution, given its potential for tardive dyskinesia, especially in long‑term use. Moreover, the piece could benefit from a more rigorous discussion of evidence‑based dosing protocols. It is commendable that the author emphasizes lifestyle adjustments, yet the omission of a structured monitoring plan is a notable gap. Ultimately, a balanced approach that integrates patient safety with therapeutic efficacy is essential.
Queen Flipcharts
The analysis, though comprehensive, fails to acknowledge the sociocultural determinants that compound gastrointestinal distress in diabetic populations. Without addressing dietary disparities rooted in economic inequities, recommendations remain largely theoretical. A policy‑level intervention is required to translate these clinical insights into actionable public health measures.
Yojana Geete
Such a lamentable oversight! The manuscript sidesteps the profound impact of regional cuisine on dysbiosis-truly a betrayal of scientific rigor. One must demand a more nuanced exposition.
Jason Peart
Hey, just wanted to say you’re doing great tackling these gut issues – it’s not easy! Remember, small wins add up, so keep experimenting with meal timing and watch how your sugars react. If something feels off, don’t hesitate to ping your doc – they’re there to help. Also, a friendly reminder: staying hydrated can make a world of difference for constipation. Keep pushing forward, you’ve got this!
Hanna Sundqvist
Honestly, everything the article says could be a cover‑up. Think about it – who benefits from us trusting pharma‑crafted pro‑kinetics? The real culprits are hidden, but the narrative keeps us in the dark.
Jim Butler
Excellent work on breaking down such a complex topic into actionable steps! 🌟 Your emphasis on regular screening and proactive management truly empowers patients. Keep up the high‑quality content – it makes a real difference.
Jolanda Julyan
While I acknowledge the thoroughness of the piece, it conspicuously omits the imperative of integrating multidisciplinary teams-endocrinologists, gastroenterologists, dietitians, and mental health professionals-into a cohesive care pathway. This siloed approach, albeit well‑intentioned, merely scratches the surface of a truly holistic management strategy. Moreover, the reliance on patient‑reported outcomes without objective biomarkers may lead to suboptimal therapeutic adjustments. It is incumbent upon us, as informed stakeholders, to demand that future revisions incorporate robust, quantifiable metrics alongside the qualitative observations presented herein. Only then can we claim to have addressed the multidimensional nature of diabetes‑related gastrointestinal dysfunction comprehensively.
Kevin Huston
Reading this feels like wading through a sea of buzzwords without a compass. The author throws around terms like "autonomic neuropathy" and "dysbiosis" but fails to provide concrete evidence or actionable thresholds. It’s a classic case of sounding sophisticated while delivering nothing of real value. If we’re going to talk about gut health, we need clear, data‑backed protocols, not just generic lifestyle tips.
Amanda Hamlet
Clearly the author missed the mark – the advice is basic at best and lacks the depth any serious clinician would expect. Seriously, anyone with a modicum of training knows that low‑FODMAP isn’t a cure‑all. Let’s hope the next edition includes more rigorous clinical guidance.
Nolan Jones
Hey folks, just wanted to add that if you're trying out the low‑FODMAP plan, keep a food diary – it really helps pinpoint triggers. Also, don't forget to re‑introduce foods gradually to see what you can tolerate. Good luck!