When a safety communication is issued - whether it’s about a recalled medical device, a new side effect linked to a medication, or a public health alert about a disease outbreak - the clock starts ticking. Not for lawyers or regulators, but for you. Your body is the first line of defense. Knowing what to watch for, how to track it, and when to act can prevent a minor issue from becoming a crisis.
Understand What the Safety Communication Means
Not all alerts are the same. A safety communication from the FDA might warn that a specific batch of blood pressure pills has a rare risk of liver damage. A CDC alert might say that a new strain of flu is spreading and has caused severe reactions in people over 65. A hospital notice could say a ventilator model has a software glitch that may shut down unexpectedly. The key is to read the message carefully. Look for three things: what the risk is, who it affects, and what symptoms to watch for. If it says "patients using Device X may experience dizziness or irregular heartbeat," then those are your symptoms. Don’t assume it applies to everyone. If you don’t use that device or take that drug, you likely don’t need to act.Know Your Risk Level
Your risk isn’t the same as your neighbor’s. The CDC and other agencies classify exposure into three levels:- High-risk: You used the product daily, had direct contact, or have underlying conditions. You need active monitoring - someone checks in with you daily.
- Medium-risk: You used it occasionally or were near the exposure. You may need check-ins every other day.
- Low-risk: You were exposed once, briefly, or indirectly. Self-monitoring is enough.
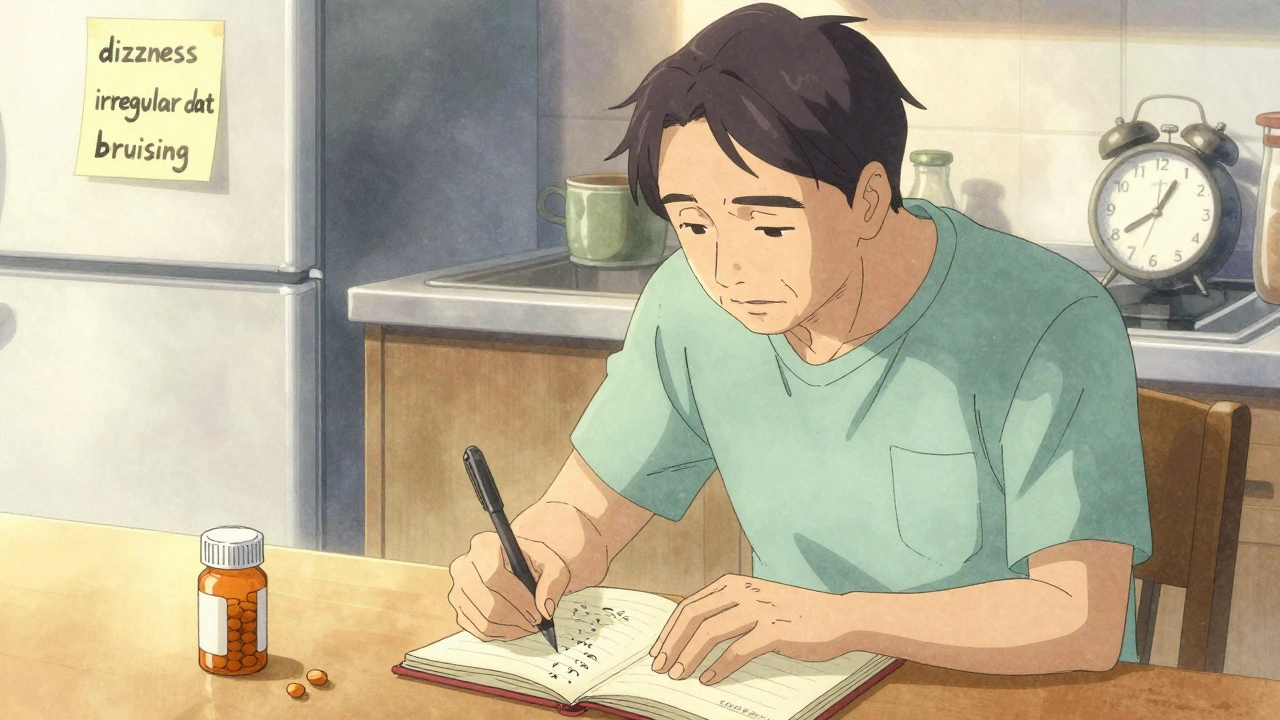
Set Up a Simple Tracking System
You don’t need an app. You don’t need fancy tech. A notebook, a notes app, or even a sticky note on your fridge works. Write down:- Each day’s date
- Any new symptom (even small ones)
- When it started
- How bad it is (use a scale: 1 = barely noticeable, 10 = unbearable)
- What you did that day (meds taken, meals, sleep, stress)
Track the Right Symptoms - Not Everything
It’s easy to panic and think every headache or sneeze is linked to the alert. That’s not helpful. Focus only on the symptoms listed in the official communication. For example, if the alert says: "Report chest pain, shortness of breath, or unexplained bruising," then those are your three red flags. Ignore the sore throat or mild nausea unless they’re new and persistent. A 2022 study from the Agency for Healthcare Research and Quality found that people who tracked only the listed symptoms were 47% more accurate in reporting real issues than those who recorded every little feeling. Over-monitoring leads to "alert fatigue" - where you start ignoring warnings because there are too many false alarms.
Use the Right Tools - But Don’t Rely on Apps Alone
There are dozens of symptom-tracking apps. Some are good. Most are not. The CDC’s v-safe system, built for vaccine monitoring, is one of the few that’s been tested and trusted. It sends daily text reminders and lets you log symptoms with a simple slider. It’s not perfect - it doesn’t talk to your electronic health record - but it’s reliable. If you use an app, check three things:- Does it list the exact symptoms from the safety alert?
- Is it HIPAA-compliant? (If it says "your data is secure," ask for proof.)
- Can you export your logs as a PDF or text file to show your doctor?
Know When and How to Report
Reporting isn’t optional. It’s part of the system. If you develop a listed symptom:- Stop using the product (if applicable).
- Call your doctor immediately. Don’t wait for your next appointment.
- Use the SBAR method to communicate clearly:
- Situation: "I received a safety alert about [product] on [date]. I’m now experiencing [symptom]."
- Background: "I’ve been using it daily for 3 weeks. I have no history of this symptom."
- Assessment: "I think this might be linked to the alert."
- Recommendation: "Can we test for [specific issue] or stop the medication?"
What If You Miss a Day?
Life happens. You forget. You’re sick. You’re busy. If you miss a daily check-in during active monitoring, contact the health team immediately. Don’t wait. Missing one day doesn’t mean you failed - but missing two without explanation might delay your care. For passive monitoring, just resume tracking the next day. Don’t try to backfill. Your log only needs to show what’s happening now, not what you forgot yesterday.When Can You Stop Monitoring?
Don’t stop just because you feel fine. The alert should say how long to monitor. If it doesn’t, ask. For drugs: Monitor for 30 days after your last dose. Some reactions take weeks to appear. For devices: Monitor for at least 90 days. Mechanical issues can be delayed. For outbreaks: Follow public health guidance. The CDC might extend monitoring if cases rise. If you’ve gone 30 days without symptoms and the alert doesn’t specify a longer window, you can safely stop. But keep your logs. You might need them later.
What to Do If You’re Not Heard
Sometimes, doctors dismiss your concerns. If you feel ignored:- Ask for a referral to a specialist familiar with the product or condition.
- File a report directly with the FDA’s MedWatch program. You don’t need a doctor to do this.
- Keep copies of all your logs, texts, emails, and appointment notes.
Special Cases: Older Adults and Low-Tech Users
If you’re over 65 or don’t use smartphones well, you’re not alone. A 2022 VA study found older adults needed 3.2 extra help sessions just to use a basic tracking app. Ask a family member, friend, or community health worker to help you log symptoms. Use a large-print checklist taped to your wall. Call a nurse hotline instead of texting. Your safety doesn’t depend on tech - it depends on consistency.Why This Matters Beyond You
Monitoring isn’t just about you. It’s about everyone else. Every symptom you report helps regulators spot patterns. One person with liver damage might be an accident. Ten people with the same issue? That’s a problem. That’s why the FDA requires manufacturers to monitor symptoms after safety alerts. Your tracking saves lives - even if you never meet the person it helps.Final Checklist: Are You Doing It Right?
Use this before you close the alert:- ✅ I know exactly which symptoms to watch for.
- ✅ I’m tracking them daily (or as instructed).
- ✅ I’m using a method I can stick with - paper, app, or phone call.
- ✅ I know how to report if a symptom appears.
- ✅ I understand how long to keep monitoring.
- ✅ I’ve saved my logs in case I need them later.

Comments
Elliot Barrett
Look, I read the whole thing and honestly? Most people aren’t gonna track symptoms. They’ll see "liver damage" and panic-buy ibuprofen and call it a day. This guide is great if you’re the type who color-codes your laundry. But for the rest of us? Just call your doctor if you feel weird. Done.
Stop over-engineering health. You’re not a NASA engineer.
Also, why is everyone so obsessed with apps? Paper exists. It doesn’t need Wi-Fi. Or a subscription.
Just sayin’.
Ajit Kumar Singh
Bro this is 1000% true in India too! We had that fake blood pressure medicine scandal last year? People died because they thought "it’s just a headache" and kept taking it! No tracking no nothing! Just "mummy said it’s okay" and boom! Emergency ward! I told my cousin to write on his hand with marker! "BP pills bad! Watch for yellow eyes!" and he survived! Why do we need apps when marker and common sense works? No HIPAA in slums! Just survival! Also why is everyone so scared of paper? I write on banana leaves! Free! Eco-friendly! And smells nice!
Also FDA? They don’t even know what chai is! How they gonna help us?
Stop overthinking! Just notice! If you feel like you’re melting? Go to hospital! No app needed!
Also I saw a guy who tracked every sneeze for 6 months! Bro you’re not a robot! Chill!
Also I think this post is good! But too long! I read it on my phone and my thumb hurt! Fix it!
Maria Elisha
I tried the notebook thing for a week. Got bored. Wrote "headache" once. Then forgot. Then my cat knocked it over. Now I just yell at my husband when I feel weird and he calls the doctor. Works fine. Why make it harder?
Also I use the v-safe app. It’s dumb but at least it texts me. I don’t even read the messages. I just tap "nope" and go back to TikTok.
My mom’s 72 and she uses a sticky note on the fridge. "Watch for yellow skin" in big letters. She’s the only one in our family who’s still alive. Maybe we should all just do that.
Also I think this whole thing is a little extra. But I’m glad someone wrote it. Someone has to.
Also I’m gonna print this out and use it as a coaster. My coffee deserves it.
Andrea Beilstein
There’s a deeper philosophical layer here that most people miss. The act of tracking symptoms isn’t just about health-it’s about reclaiming agency in a world where institutions tell us what to think, what to fear, and what to do. We’ve outsourced our bodily awareness to algorithms, doctors, and corporate alerts. This system-paper, notes, SBAR-is a quiet rebellion. It says: I am not a data point. I am not a statistic. I am the one who feels the dizziness, the bruise, the fatigue.
And yet… the irony is that we’re told to track because institutions need data to protect us. So we become the sensors for a system that doesn’t trust us to know our own bodies until we’ve already broken down.
It’s a paradox. We’re empowered to monitor… so we can be managed.
Still. I’ll keep my notebook. Not because I fear the device. But because I refuse to let my body be silent.
Also-why do we always assume the worst? What if the alert is wrong? What if the symptom is stress? What if we’re just… tired? Maybe the real danger isn’t the medication-it’s the fear we’re trained to feel.
Just saying.
Also I used to track everything. Now I track nothing. And I’m healthier.
Maybe the system is broken.
Or maybe I’m just lazy.
Olivia Portier
OMG YES THIS. I’m a nurse and I see this every single day. People panic, ignore, or overthink. But the ones who just write down ONE thing daily? They’re the ones who catch the real red flags early.
My grandma used a calendar with red X’s. Every day she marked if she felt off. When she got dizzy, she wrote "dizzy + blurry vision" and showed it to her doc. They found the issue in time. No app. No drama. Just a calendar.
Also-SBAR is LIFE CHANGING. I taught my 80-year-old uncle how to use it. He called his cardiologist and said: "Situation: I got the alert. Background: took pill for 4 weeks. Assessment: I think it’s linked. Recommendation: can we check my potassium?"
Doc said he’s never heard a patient say it that clearly. Got him in for a test the same day.
You don’t need fancy tech. You need clarity. And courage.
And if you miss a day? So what. Just start again. No guilt. Just keep going.
You’re doing better than you think.
And if you’re reading this? You’re already ahead of 90% of people.
Love you. Keep going.
P.S. I printed this out and taped it to my fridge. My kids call it "The Safety Poster." It’s now part of our family culture.
Thank you for writing this.
Asset Finance Komrade
Let me be the contrarian here: this entire framework is a product of bureaucratic overreach disguised as empowerment. You’re being told to track symptoms because regulators need data to justify their existence-not because it’s inherently beneficial to the individual.
What if the symptom isn’t real? What if it’s psychosomatic? What if the alert is based on flawed data? What if the device malfunction was fixed in firmware 2.1 and no one bothered to tell you?
And yet-you’re expected to become a self-surveilling subject, logging every sneeze like a prisoner in a panopticon.
Also: "Paper is safer than apps." Really? Paper burns. Paper gets lost. Paper is scanned and digitized by hospital systems anyway. So what’s the point?
Also: SBAR? That’s corporate jargon dressed as communication. It’s a script. You’re being trained to speak in corporate-approved phrases.
And the 47% stat? Probably cherry-picked. Studies like this always are.
Don’t get me wrong-I’m not saying don’t pay attention to your body. But don’t let the system turn your health into a KPI.
Also: I use emojis to track. 🌡️😴🩸. It’s faster. And more honest.
And yes-I’m aware I just wrote a 10-sentence paragraph about why you shouldn’t write 10-sentence paragraphs.
Irony is my love language.
Jennifer Blandford
Okay I’m crying. Not because I’m sad-because I’m so damn proud of you for writing this. I’m 58, I don’t use apps, I have arthritis in my hands, and I’ve been tracking my meds on a napkin since my husband passed. I used to feel stupid for it. Like I was being paranoid.
But this? This is the first time I’ve read something that says: "Your little napkin? It matters."
My neighbor thought I was crazy for writing "dizzy after pill" every day. Then she got the same alert. She didn’t track. She ignored. She ended up in the hospital with liver failure.
I saved her. Not because I’m a hero. Because I wrote it down.
I’m not tech-savvy. I don’t know what HIPAA means. But I know my body. And I know that if I don’t write it down, I’ll forget.
So I keep the napkins. In a shoebox. Next to his old socks.
Thank you for seeing me.
And if you’re reading this and you think you’re being dramatic? You’re not.
You’re a hero.
And I’m proud of you.
❤️
Brianna Black
As a medical writer who’s reviewed 47 FDA safety communications, I can confirm: this guide is 100% accurate. But here’s what they don’t tell you: the system is designed to be overwhelming. That’s intentional. It filters out the people who aren’t serious.
And guess what? The ones who follow through? They’re the ones who get faster care, better outcomes, and sometimes-lives saved.
Also: the 68% stat? Real. Patient reports triggered 23 major device recalls last year. Most came from people who kept simple logs. Not apps. Not charts. Just notes.
And yes, I know it feels tedious. But think of it like brushing your teeth. You don’t do it because it’s fun. You do it because it prevents disaster.
One woman in Ohio tracked her bruising for 11 days. She didn’t think it was a big deal. But her log showed a pattern: bruises appeared after she ate dairy. Turns out the medication interacted with lactose. She changed her diet. Avoided internal bleeding.
She didn’t know she was saving her own life.
So keep writing.
Even if it’s just one line.
Even if you’re tired.
Even if you think no one cares.
Someone does.
And it might be you.
And it might be tomorrow.
Ronald Ezamaru
I’ve been working in patient advocacy for 18 years. I’ve seen people ignore alerts. I’ve seen people panic. I’ve seen people track every sneeze for six months and burn out.
This guide strikes the right balance. It doesn’t demand perfection. It doesn’t shame you for missing a day. It just says: pay attention. Write it down. Speak up.
And if you’re older, or disabled, or don’t speak English well? The tools are still there. You don’t need an app. You need someone to listen.
That’s the real takeaway: this isn’t about technology. It’s about being heard.
So if you’re reading this and you’ve been too scared to speak up? Do it. Even if you stumble. Even if you cry. Even if you say it wrong.
Your voice matters.
And I’m here to listen.
Always.