Every year, thousands of children are given the wrong dose of medicine-not because someone was careless, but because a simple number was wrong. A weight written in pounds instead of kilograms. A calculation done on a napkin. A scale that hasn’t been calibrated in months. These aren’t rare mistakes. They’re systemic failures-and they’re preventable.
Why Weight-Based Checks Are Non-Negotiable in Pediatrics
Children aren’t small adults. Their bodies process medicine differently. A dose that’s safe for a 70-pound teen could be deadly for a 14-pound infant. That’s why every pediatric medication dose must be calculated based on weight-usually in milligrams per kilogram (mg/kg). But here’s the problem: 15% to 20% of pediatric medication errors come from weight conversion mistakes, according to the American Society of Health-System Pharmacists (ASHP, 2018). In one study, 32.7% of all dispensing errors in children involved incorrect weight-based calculations. And 8.4% of those caused real harm.
The CDC’s PROTECT Initiative found that 40% of liquid medication errors in kids under 4 happened because someone mixed up pounds and kilograms. Imagine a parent handing over a prescription for 10 mL of amoxicillin, thinking it’s for a 22-pound baby. But the chart was written in kilograms-so the actual weight was 10 kg. That’s a 100% overdose. This isn’t theoretical. It’s happening in clinics, hospitals, and even community pharmacies every day.
The Three Critical Points of Verification
There’s no single fix. Preventing these errors requires checking weight at three key moments: when the order is written, when the pharmacy fills it, and when the nurse gives it to the child.
1. Prescription Entry
If the doctor doesn’t enter the correct weight in kilograms before ordering, nothing else matters. Electronic Health Record (EHR) systems must block prescription submission until weight is entered. No exceptions. Systems like Epic’s Pediatric Safety Module 4.0 (released in January 2024) now use growth percentiles-not just static weight-to flag suspicious doses. If a 12-year-old weighs 45 kg but the system suggests a dose meant for a 20 kg child, it alerts the prescriber. That’s smart design.
2. Pharmacy Verification
Pharmacists aren’t just filling bottles. They’re the last line of defense. Every weight-based calculation must be independently verified by a second pharmacist. No shortcuts. A 2021 study showed pharmacist-led verification reduced administration errors by 15.8 percentage points. But it takes resources: 2.5 full-time pharmacists per 100 pediatric beds. That’s expensive. But not as expensive as a child’s liver failing from an acetaminophen overdose.
3. Bedside Administration
Barcode scanning isn’t just for adult wards. When a nurse scans a child’s wristband and the medication, the system should cross-check the weight, dose, and concentration. If they don’t match, the system should stop the process. A 2020 study found this step cut administration errors by 74.2%. Yet, only 32.7% of rural hospitals have this tech. That’s a dangerous gap.
Technology That Actually Works
Not all tech helps. Some systems create more noise than safety.
Computerized Provider Order Entry (CPOE) with built-in clinical decision support cuts prescribing errors by 87% compared to paper orders, according to a 2014 meta-analysis. But standalone tools-like printed dosing charts-only reduce errors by 47% in complex settings. Why? Because they don’t talk to the EHR. They’re static. A child’s weight changes. A chart doesn’t.
Automated dispensing cabinets with weight-based checks cut errors by nearly 70%. But they add 2.3 minutes per prescription. That’s a trade-off. Some nurses hate it. But when a child nearly died from a tenfold overdose because the cabinet didn’t flag it, the extra time feels worth it.
Here’s the catch: alert fatigue. A 2021 study found 41.7% of weight-based alerts were ignored. And 18.3% of those ignored alerts were real errors. That’s not just annoying-it’s deadly. The fix? Better rules. Epic’s new system uses growth curves, not fixed numbers. If a child’s weight is in the 95th percentile, the system adjusts the upper limit. Fewer false alarms. More trust.

Standardization Is the Silent Hero
One of the biggest hidden causes of errors? Inconsistent concentrations. One hospital uses 250 mg/5 mL of amoxicillin. Another uses 400 mg/5 mL. Nurses and pharmacists get confused. A 2023 study found that standardizing concentrations reduced calculation errors by 72.4%.
So what’s the standard? The American Academy of Pediatrics says: use milliliters only. No teaspoons, no tablespoons. No “a dropperful.” Just mL. And every label must say: “Dose based on weight: ___ mg/kg.”
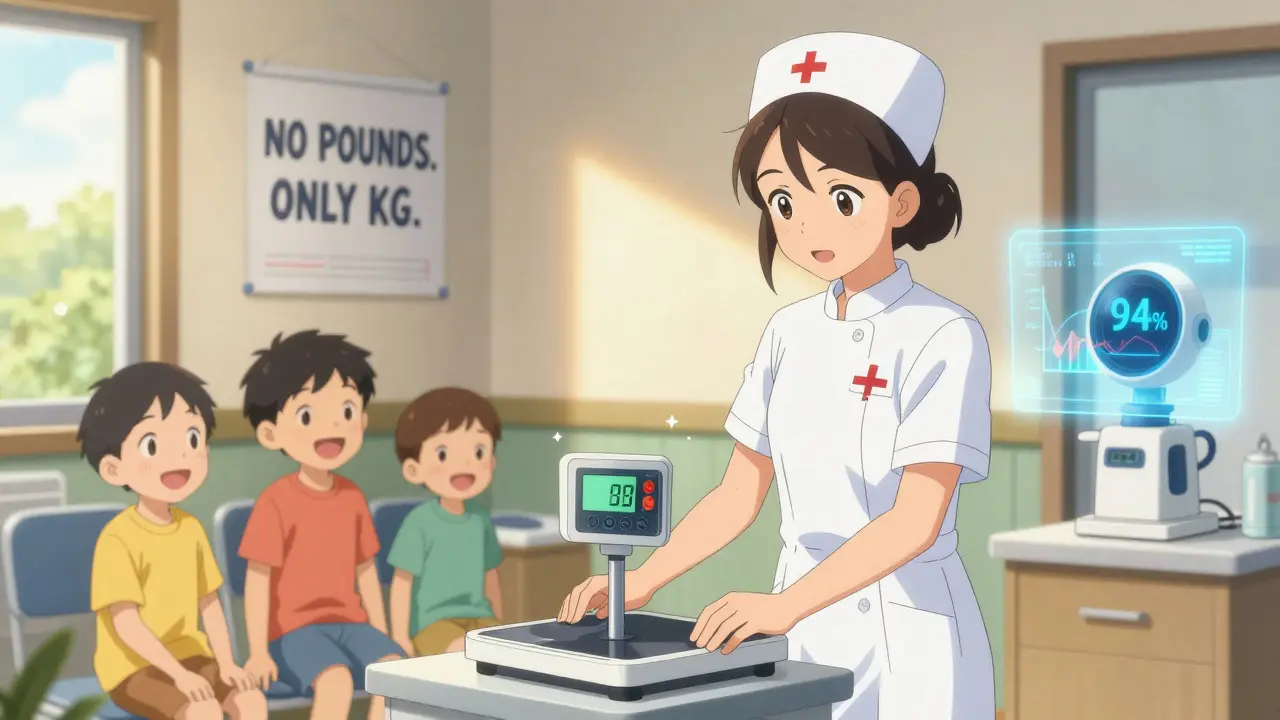
Also, ditch pounds. All weights must be documented in kilograms. Period. ASHP made this mandatory in 2018. Digital scales should display only kg-with 0.1 kg precision for infants, 0.5 kg for older kids. If your scale shows pounds, it’s outdated. Replace it.
What Happens When You Don’t Do This
At Boston Children’s Hospital, before they mandated kilogram-only weights, they had 14.3 weight-related errors per 10,000 doses. After implementation? 0.8. That’s a 94% drop.
But not everywhere is so lucky. Community pharmacists without EHR access report 28.4% have had a weight-related near-miss in the past month. In rural hospitals, only 32.7% have full weight-based systems. Meanwhile, academic centers hit 94.3%. That’s not equity. That’s a safety crisis.
And it’s getting worse. A 2022 survey found 63.2% of pediatric nurses had seen weight documentation errors in the past year. Over 40% said those errors caused medication delays. Kids waited. Parents panicked. Nurses burned out.
Implementation Is Hard-But Not Impossible
Setting this up takes time, money, and culture change.
ASHP recommends a 6-9 month rollout. That includes:
- Training every clinician for 40 hours on pediatric pharmacokinetics
- Configuring EHRs to require weight before any order can be placed
- Standardizing all liquid medications to one concentration per drug
- Installing digital scales that show only kilograms
- Adding dual verification steps in pharmacy
- Integrating weight data into barcode scanning systems
And you need staff. 1.5 full-time pharmacists per 50 pediatric beds. That’s not optional. It’s the cost of safety.
Resistance? Yes. Doctors say it slows them down. Nurses say the alerts are annoying. But when a child survives because a system caught a 10x overdose? That’s the moment everyone remembers why it matters.
The Future Is Smarter-But Still Human
The FDA is pushing for EHRs to integrate growth charts to flag doses that don’t match age and weight trends. AI tools are being tested to predict a child’s expected weight based on past data. One pilot system got 92.4% accuracy spotting outdated weights.
Blockchain for weight records? Real-time monitoring via wearables for kids with chronic illnesses? These are coming. But none of it matters if the culture doesn’t change.
As Dr. Robert Wachter from UCSF said: “Technology alone cannot prevent errors. A culture of safety with non-punitive error reporting is essential.”
That means: if a nurse reports a near-miss, they’re not fired. They’re thanked. If a pharmacist catches a wrong dose, they’re celebrated. If a doctor forgets to enter weight, the system reminds them-without shame.
Because in pediatrics, the smallest mistakes have the biggest consequences. And the fix isn’t fancy. It’s simple: weight-based checks. At every step. Every time. No exceptions.
What You Can Do Today
You don’t need a $2 million EHR upgrade to start protecting kids.
- Ask your facility: Are all weights documented in kilograms?
- Check if scales show pounds. If yes, demand new ones.
- Verify that every pediatric prescription requires weight before submission.
- Ask pharmacists: Do they double-check every weight-based dose?
- Push for standard concentrations for common meds like amoxicillin and acetaminophen.
- Report any near-miss. No blame. Just learn.
One wrong dose can change a child’s life forever. But one good check can save it.
Why is weight in kilograms mandatory for pediatric dosing?
Weight must be in kilograms because all pediatric medication dosing formulas are calculated in mg/kg. Using pounds creates unnecessary conversion steps, which are error-prone. The American Society of Health-System Pharmacists (ASHP) made kilogram-only documentation mandatory in 2018 to eliminate the 12.6% of errors caused by pound-to-kilogram mistakes. Digital scales must display only kilograms to prevent confusion.
How often should a child’s weight be re-measured?
For acute care settings, weight must be measured within 24 hours of admission. For outpatient or chronic care, it must be updated every 30 days. The Institute for Safe Medication Practices (ISMP) warns that outdated weights are the leading cause of verification system failures. If a child has gained or lost significant weight, the dose must be recalculated-no matter what the old chart says.
Can automated systems replace human verification?
No. Automated systems reduce errors by up to 87%, but they can’t replace human judgment. Alerts can be wrong. Data can be outdated. A pharmacist’s trained eye catches what software misses-like a child who’s underweight for their age, or a dose that looks right but is for the wrong condition. Technology is a tool, not a replacement. The best systems combine smart tech with mandatory dual verification.
Why do some pharmacists ignore weight-based alerts?
Alert fatigue. Many systems trigger too many false positives-especially for adolescents approaching adult weight ranges. If an alert pops up 10 times a shift and 9 of them are wrong, people stop paying attention. The solution is smarter rules: using growth percentiles, adjusting dose limits dynamically, and reducing unnecessary alerts. Training staff to understand why alerts matter also helps.
What’s the biggest barrier to implementing weight-based checks in small hospitals?
Lack of integrated EHR systems and funding. Only 32.7% of rural hospitals have full weight-based verification systems, compared to 94.3% of academic children’s hospitals. Without EHR integration, pharmacists can’t verify weights in real time. Many can’t afford digital scales, training, or extra staff. Policy changes like CMS’s 2024 requirements and Leapfrog’s safety grades are pushing change-but progress is slow where resources are thin.
Are there legal consequences for not using weight-based verification?
Yes. CMS now requires weight verification documentation for all pediatric Medicare/Medicaid prescriptions under its 2024 Hospital Outpatient Prospective Payment System. The Leapfrog Group includes weight verification as a required element for a hospital’s ‘A’ safety grade. Failure to comply can mean lost funding, lower ratings, and increased liability in malpractice cases. In 2023, a hospital paid $1.2 million in settlement after a child suffered brain damage from a weight-based dosing error.


Comments
Robert Way
so i just saw a kid get the wrong dose at my cousin's hospital and it was because the nurse typed in 22 lbs instead of 10 kg... and no one caught it till the mom asked why the baby was so sleepy. like bro, we got computers for this. why are we still writing on napkins?
TooAfraid ToSay
oh wow so now we’re making doctors and nurses into data entry clerks? next they’ll make us weigh the kids with a blockchain scale. this is just bureaucratic theater. the real problem? lazy parents who don’t know how to read a scale. fix the people, not the system.
Dylan Livingston
Let me just say, as someone who has read every single guideline from ASHP, CDC, AND the AAP, this post is charmingly naive. You think standardizing concentrations and forcing kg-only weights is the answer? Darling, you’re missing the forest for the trees. The real issue is that pediatric pharmacology is still treated like an afterthought in medical education. We train doctors to treat adults, then throw them into pediatrics and say ‘good luck.’ No one teaches them how to think in mg/kg. No one. And now you want a digital scale to fix that? Sweetheart, the problem is epistemological, not technical.
shiv singh
in india we dont even have digital scales in most clinics. some places still use old balance scales with metal weights. and you want us to switch to kg? first teach the staff what kg even means. i saw a nurse ask a mom 'is your baby 10 or 100?' like it was a riddle. this is not a tech problem. its a poverty problem.
Vicky Zhang
I just want to say thank you for writing this. I’m a pediatric nurse and I’ve seen too many near-misses. Last month, a toddler almost got 10x the right dose because the chart said 22 lbs and the med was dosed for kg. I caught it because I always double-check. But I shouldn’t have to be the hero. This system should catch it before I even open the bottle. Please, hospitals - stop treating safety like an optional bonus. It’s the foundation.
Allison Deming
It is imperative to underscore the legal ramifications of noncompliance with weight-based verification protocols. As delineated in the 2024 CMS Hospital Outpatient Prospective Payment System, failure to adhere to standardized pediatric dosing procedures constitutes a breach of the standard of care. Consequently, institutions may face significant financial penalties, diminished Leapfrog ratings, and increased exposure to malpractice litigation. The moral imperative is clear, but the legal obligation is unequivocal.
Andrew Freeman
kg only? lol sure. next they’ll make us use latin for prescriptions. i’ve seen nurses write ‘5 ml’ as ‘5mL’ and then argue over it for 10 minutes. we dont need more rules. we need people who can count. and maybe stop hiring people who think ‘pounds’ is a type of sandwich.
says haze
Let’s be honest - this whole ‘weight-based check’ movement is just another neoliberal technofix for a system that refuses to fund proper staffing. You want fewer errors? Hire more pharmacists. Pay nurses more. Stop treating healthcare like a startup that needs to ‘optimize.’ The real tragedy isn’t the pound-to-kilo mistake - it’s that we’ve normalized working in a broken system and call it ‘safety culture.’ You can’t algorithm your way out of underfunding.
Sarah -Jane Vincent
you think this is about weight? nah. this is about the pharmaceutical industry pushing the same drugs in the same concentrations everywhere. they don’t care if it’s safe for kids. they care about profit. and the EHR companies? they sell you a system that flags ‘suspicious doses’ but won’t tell you if the drug itself is even approved for pediatric use. this whole thing is a distraction. ask yourself - why are we giving toddlers adult-strength meds in the first place?
Henry Sy
man i used to work in a rural ER and we had one scale that was older than my ex. it showed pounds, had a crack in the screen, and once gave a 140-lb reading for a 9-month-old. we just guessed. then one night a kid got too much morphine because the doc thought he was 40 lbs and he was 18. he lived. but i haven’t slept right since. this isn’t policy. this is survival.
Anna Hunger
While I commend the emphasis on procedural rigor, I must respectfully note that the implementation of mandatory dual verification requires not only institutional investment but also a redefinition of professional roles. The current model of pharmacy verification is predicated on a staffing ratio that is unsustainable in most community settings. A more equitable solution would involve cross-training nurses in basic pharmacokinetic calculations and integrating real-time clinical decision support into mobile devices - not merely relying on static EHR alerts.
Jason Yan
Hey - I get that systems and scales matter. But I’ve been doing this for 20 years, and the real magic happens when someone slows down and just talks to the parent. Not the chart. Not the computer. The mom. The dad. They’ll tell you their kid’s been sick for three days, lost weight, isn’t eating. That weight on the screen? Might be from last month. I’ve saved kids just by asking, ‘Hey, how’s he been doing at home?’ Tech helps. But humans remember what machines forget.