Every year, thousands of people in the U.S. take the wrong medication or the wrong dose because of a simple mistake on a pharmacy label. It’s not because pharmacists are careless-it’s because mistakes happen even in the best systems. A 2019 study found that 16-20% of all medication errors in community pharmacies come from labeling mistakes. And here’s the scary part: pharmacy labeling error is often the last step before harm. You might trust the pharmacy, but you’re the final safety net. If you don’t check, no one else will.
What to Look for on Your Prescription Label
Your label has five critical pieces of information. Missing or wrong details on any one of them can be dangerous. Don’t just glance-read each one out loud.- Medication name - Is it written clearly? Is it the brand name (like Lipitor) or generic (atorvastatin)? Both should be there. Look for tall-man lettering-where parts of similar drug names are capitalized to show differences, like GLIpiZIDE vs. glyBURide. This helps prevent mix-ups between drugs that sound alike.
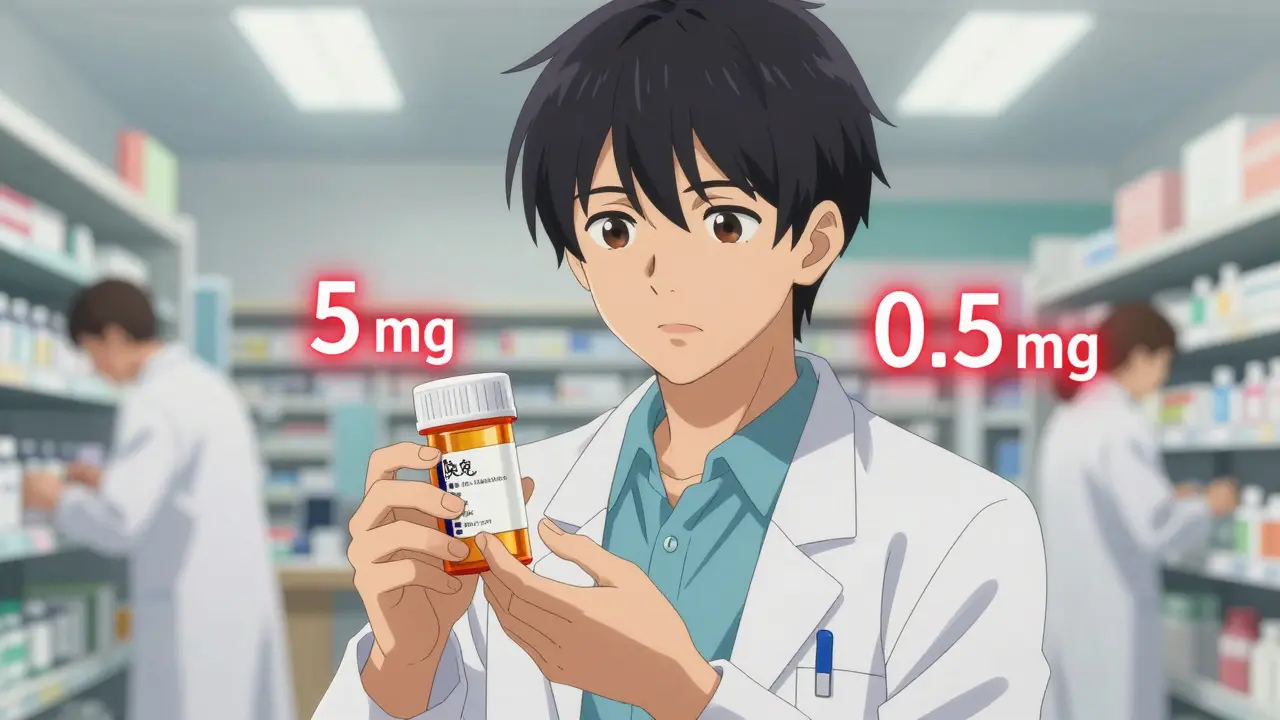
- Strength - Is it 5 mg or 0.5 mg? A decimal point out of place can turn a safe dose into a deadly one. Warfarin, insulin, and levothyroxine are high-risk medications where a 10x overdose has killed people. Read the number aloud. If it sounds off, it probably is.
- Dosage form - Is it a tablet, capsule, liquid, or patch? Getting a pill when you were supposed to get a liquid can be dangerous, especially for children or people who can’t swallow pills.
- Directions - Does it say “take one tablet by mouth once daily” or “take one tablet by mouth three times daily”? If the directions don’t match what your doctor told you, ask. A study showed patients who compared new labels to their doctor’s instructions caught 92% of errors.
- Indication - Why are you taking this? This is the most overlooked part. Only 18% of community pharmacy labels include it. But if your label says “for high blood pressure” and your doctor told you it’s for diabetes, that’s a red flag. Research shows including the indication helps patients spot wrong medications 63% more often.
Common Labeling Errors You Can Catch
Some mistakes happen over and over. Here are the top three-and how to spot them.Look-alike, sound-alike (LASA) drugs - These are drugs with names that sound or look too similar. The FDA lists over 1,500 risky pairs. Cycloserine and cyclosporine? One treats tuberculosis, the other suppresses your immune system after a transplant. Mix them up, and you could get seriously sick. Look for tall-man lettering. If it’s not there, ask the pharmacist to write it in.
Dosage form errors - A patient in Texas once took a liquid antibiotic meant for a child, thinking it was a pill. She ended up in the ER. Always check if it’s a tablet, capsule, syrup, or patch. If the shape or texture doesn’t match what you’ve taken before, don’t assume it’s the same.
Strength errors - These are the deadliest. A woman in Michigan took 5 mg of warfarin instead of 0.5 mg. She bled internally and nearly died. The label said “5 mg” with no decimal point. That’s a classic error. Always read numbers aloud. Say “zero point five milligrams,” not “point five.” Say “five milligrams,” not just “five.” Your brain catches mistakes better when you hear them.
How to Verify Like a Pro
The Agency for Healthcare Research and Quality (AHRQ) created a simple 4-step check that works every time. It takes less than two minutes.- Compare to your prescription - Did your doctor write “metformin 500 mg twice daily”? Does the label match? If you’re not sure what your doctor prescribed, call them or check your portal. Most doctors now send e-prescriptions-log in and compare.
- Use tall-man lettering - If the label says “PROMETHAZINE” and “PREMAZINE,” the capitalized letters are meant to help you see the difference. If it doesn’t, ask the pharmacist to highlight it with a pen.
- Read the strength out loud - Say it like this: “Zero point two five milligrams.” Don’t say “point two five.” Say “five milligrams,” not just “five.” Hearing it makes your brain catch the mistake.
- Confirm the reason - “Why am I taking this?” If the label says “for anxiety” but you were prescribed it for high blood pressure, stop. Ask. This step alone catches nearly two out of every three wrong-medication errors.
Pharmacists at Mayo Clinic started requiring patients to say the purpose of their medication before leaving the pharmacy. That “teach-back” method cut labeling errors that reached patients by 68%. You don’t need to be a doctor-you just need to speak up.
High-Risk Medications to Double-Check
Some drugs are more dangerous if mislabeled. If you’re taking any of these, spend an extra 30 seconds verifying:- Insulin - Wrong type or dose can cause coma or death
- Warfarin (Coumadin) - A small change in dose can cause bleeding or clots
- Levothyroxine - Too much can cause heart problems; too little won’t help your thyroid
- Hydralazine vs. Hydroxyzine - One lowers blood pressure, the other treats allergies
- Glipizide vs. Glyburide - Both treat diabetes, but one lasts longer and can cause low blood sugar
- Opioids (oxycodone, morphine) - Wrong dose can cause breathing failure
These six medications account for 65% of serious outcomes from labeling errors, according to the FDA’s 2021 report. If you’re on any of them, treat every refill like it’s your first time.
Why You Can’t Rely on the Pharmacy Alone
Pharmacists are trained, but they’re busy. One study found that even pharmacist double-checks miss 3.4% of errors. In community pharmacies, where most people get their meds, staff often handle 150+ prescriptions a day. That’s one every 20 seconds. Mistakes happen.Barcodes and automated systems reduce errors by 86%-but only 32% of community pharmacies use them. Hospitals use them 78% of the time. That’s why hospital pharmacies have 35% fewer labeling errors.
And here’s the truth: most people don’t check. A 2022 Consumer Reports survey found only 37% of patients verify their labels every time. Why? 58% said they “trust the pharmacy.” 32% said they “didn’t know what to check.” Trust isn’t safety. Ignorance isn’t protection.
What’s Changing to Help You
Good news: things are improving. Starting May 1, 2024, new U.S. Pharmacopeia (USP) rules require all pharmacy labels to use:- Minimum 12-point font size
- 4.5:1 contrast ratio (black text on white, not gray on white)
- Standardized tall-man lettering for 200 high-risk drug pairs
- Indication for use on every label
Also, new apps like MedSafety Check let you scan your label with your phone. It compares the text to the correct drug profile and alerts you if something’s wrong. It’s 94.7% accurate.
CVS now offers “Label Lens” in over 5,200 stores. Scan the QR code on your bag, and your phone plays an audio description of the medication. No reading required.
And the federal government just passed the Patient Medication Safety Act, funding $150 million for patient education programs. Training modules are being tested in 200 pharmacies right now.
What to Do If You Find a Mistake
Don’t take the medication. Don’t argue. Don’t feel embarrassed.Call the pharmacy. Say: “I think there’s an error on my label. The strength says 5 mg, but my doctor prescribed 0.5 mg. Can you double-check?”
Most pharmacists will thank you. In fact, a Reddit thread with 147 comments found that 68% of people who reported a labeling error were thanked by the pharmacist. One user caught a 10-fold warfarin error-saved from internal bleeding.
If the pharmacy denies it, call your doctor. Or go to another pharmacy. Better safe than sorry.
Final Thought: You’re the Last Line of Defense
No system is perfect. Not the doctor. Not the pharmacist. Not the computer. The last person to see your medication before you take it… is you. And you have the power to stop a mistake before it hurts you.It takes 90 seconds. It’s not complicated. Just read the label. Say it out loud. Compare it to what your doctor told you. If something doesn’t feel right-it isn’t.
Don’t wait for someone else to fix it. Fix it yourself.

Comments
Lydia H.
Been there. Got the scary ER visit. Took my grandma's blood pressure med by accident once-thought it was mine. Turned out the label had 'Hydralazine' but the bottle said 'Hydroxyzine'. I didn't catch it till I felt my heart racing. Now I read everything out loud. Seriously, if you're not saying it, you're not seeing it.
Astha Jain
lol so u mean like if ur label says 5mg but u thought it was 0.5mg u shud just… ask? wow who knew pharmacies rnt perfect? also why is everyone so scared of decimal points? i mean its just a dot right?
Lewis Yeaple
While the intent of this article is commendable, it lacks critical nuance regarding the legal and regulatory frameworks governing pharmacy labeling in the United States. The U.S. Pharmacopeial Convention (USP) standards referenced are non-binding unless adopted by state boards of pharmacy. Moreover, the assertion that 'only 32% of community pharmacies use barcode systems' is misleading-many rely on vendor-integrated systems that do not require standalone hardware. The data cited from Consumer Reports (2022) is not peer-reviewed and suffers from selection bias. A more rigorous approach would involve referencing the National Academy of Medicine's 2018 report on medication safety.
Malikah Rajap
OMG, I just realized-I’ve never checked the INDICATION on my label… and I’ve been on levothyroxine for 8 years?!?! I mean, I know why I’m taking it, but… what if they switched me to something else?!! I’m going to the pharmacy tomorrow. And I’m going to say it out loud. Like, ‘I am taking this because… my thyroid is sad.’ I’m gonna cry. But also, thank you. I feel seen.
sujit paul
Of course they don’t put the indication on the label. The pharmaceutical-industrial complex doesn’t want you to know what you’re really taking. They profit from confusion. Why do you think they removed the old warning labels? To keep you docile. The FDA is complicit. And don’t get me started on the QR codes-those are tracking devices disguised as safety tools. Your phone is watching you. Scan the label, and they know your blood pressure, your mood, your habits. They’re building a database. You’re a data point.
Aman Kumar
The entire premise of this post is fundamentally flawed. You’re placing the burden of pharmaceutical safety on the layperson, while systemic failures-understaffing, inadequate training, profit-driven automation-are left unaddressed. This is victim-blaming dressed as empowerment. You don’t need to ‘speak up’-you need structural reform. The fact that we’ve normalized ‘checking your own meds’ as a civic duty is a moral failure of the healthcare system. And yet, here we are, turning medication safety into a self-help checklist. Pathetic.
Jake Rudin
It’s funny… I’ve been reading labels out loud since I was 12, after my dad almost took his neighbor’s insulin. He thought it was his. He didn’t know the difference between ‘Humalog’ and ‘Lantus.’ I still do it. Every time. Even if I’m alone. Even if I’m in a hurry. I say it. I hear it. I feel it. It’s not about trust-it’s about ritual. And rituals save lives.
Phil Hillson
So… I just read this whole thing and now I’m terrified. Like, full-on panic. I think I took the wrong pill last week. I’m pretty sure. I don’t know. I didn’t check. I’m gonna die. I’m already dying. I can feel it. My heart is racing. I’m gonna need a therapist. And a new pharmacist. And maybe a new life.
Josh Kenna
Y’all are overthinking this. I just hold the bottle up to the light and squint. If the letters look right, I’m good. Also, I always ask the pharmacist if it’s the same as last time. They always say yes. And I believe them. I mean, they’re the professionals. But hey, if you wanna read everything out loud, go for it. I’m just trying to get through my day without a panic attack.
Erwin Kodiat
I’m from India, and we don’t have fancy pharmacy labels here. Sometimes the script is handwritten. Sometimes the name is in three languages. But you know what? People still survive. We ask. We talk to each other. We show our labels to neighbors. We don’t wait for a USP rule. We just… care. Maybe the real solution isn’t more fonts or QR codes-it’s community. You don’t need an app to be safe. You just need someone to ask, ‘Hey, what’s this for?’
Valerie DeLoach
This is one of the most important public health messages I’ve read in years. The fact that only 18% of labels include the indication is unconscionable. And the ‘teach-back’ method used by Mayo Clinic? That’s evidence-based, patient-centered care at its finest. We need to mandate this nationwide-not as an option, but as a standard. Also, thank you for including tall-man lettering. So many people don’t know what that is. This should be required reading in every high school health class.
Christi Steinbeck
STOP WAITING. Just stop. If you’re on warfarin, insulin, or levothyroxine-you have 90 seconds to save your life. Do it now. Don’t wait for tomorrow. Don’t wait until you feel ‘ready.’ Grab your bottle. Say it out loud. Compare it. Call your doctor. You’re not being paranoid-you’re being powerful. I did it last month. Saved myself. You can too. Go. Now. I believe in you.