Every year, thousands of medication errors happen because two drug names look or sound too similar. A patient gets prednisone when they were supposed to get prednisolone. Another gets hydromorphone instead of morphine. These aren’t typos. They’re visual traps. And they can kill.
Tall-man lettering is one of the simplest, cheapest, and most effective tools we have to stop this. It doesn’t require new machines, extra staff, or expensive software. It just changes how drug names appear on screens, labels, and prescriptions - using capital letters to highlight the parts that matter most.
What Is Tall-Man Lettering?
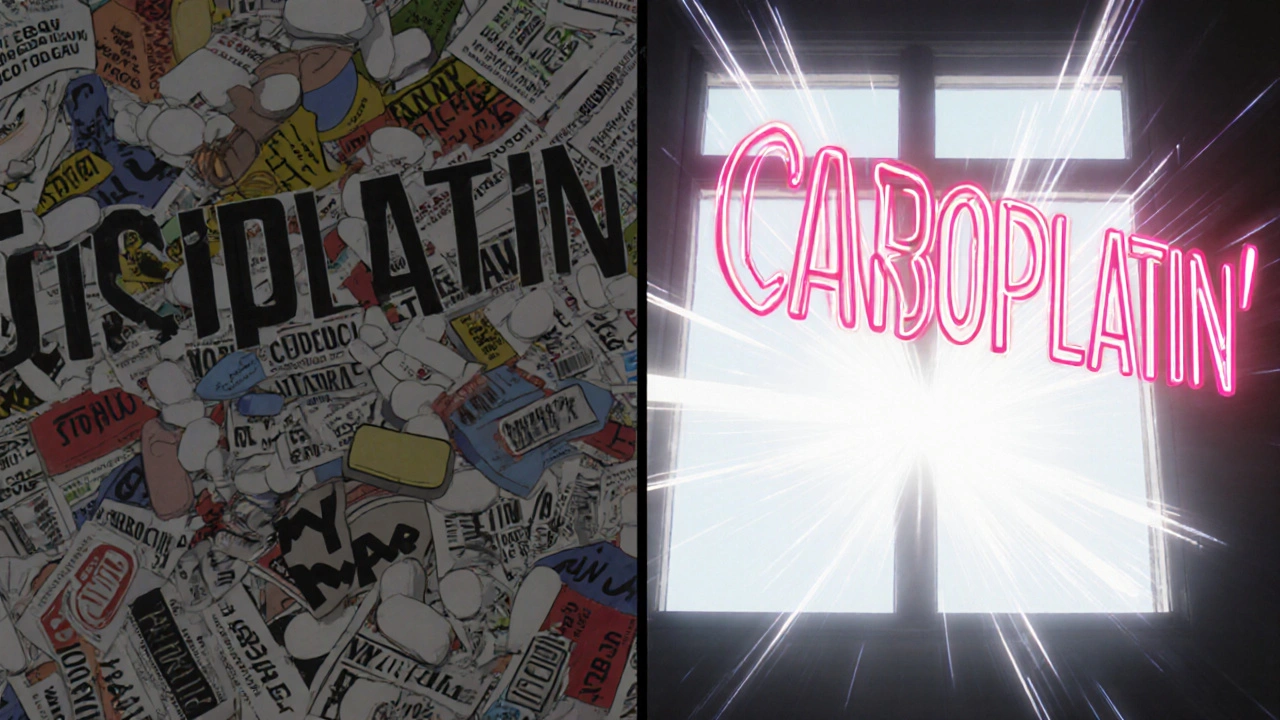
Tall-man lettering (sometimes called tallman lettering) is a way of writing drug names with selective uppercase letters to make look-alike, sound-alike (LASA) drugs easier to tell apart. For example:
- predniSONE vs. predniSOLONE
- vinBLAStine vs. vinCRIStine
- CISplatin vs. CARBOplatin
- HYDROmorphone vs. morphINE
The uppercase letters aren’t random. They highlight the key differences - the letters that change the drug’s identity. When you see SONE vs. SOLONE, your brain doesn’t have to guess. It sees the difference immediately.
This technique was developed by the Institute for Safe Medication Practices (ISMP) in 1999. The U.S. Food and Drug Administration (FDA) started officially recommending it in 2001. Today, it’s used in hospitals, pharmacies, and clinics across the U.S., Australia, New Zealand, and parts of Europe.
Why Does It Work?
Our brains are wired to recognize patterns quickly - especially in fast-paced environments like emergency rooms or busy pharmacies. When you’re scanning a list of 50 drug names, your eyes skip over lowercase letters. But uppercase letters jump out.
A 2004 eye-tracking study by ISMP showed that when pharmacists saw drug names in tall-man lettering, they made 35% fewer selection errors than when the names were in all lowercase. That’s not theoretical. That’s real people avoiding real mistakes.
It’s not about changing how drugs work. It’s about changing how we see them.
Consider this real example: A nurse in a pediatric unit almost gave a child ALPRAZolam instead of LORazepam. Both are sedatives. Both are used for anxiety. Both are spelled with 8 letters. But the difference? One has ALPRAZ, the other has LOR. If the system showed ALPRAZolam and LORazepam, the capitalization makes the difference impossible to miss.
Who Decides Which Letters to Capitalize?
There’s no single global rule. Different agencies have different lists - and that’s a problem.
The FDA has a list of 72 drug name pairs that require tall-man lettering. ISMP has a much larger list - 252 pairs - updated every quarter. Australia uses its own list of 192 pairs. The problem? They don’t always agree.
For example:
- ISMP recommends: HYDROcodone vs. oxyCODONE
- FDA recommends: HYDROmorphone vs. morphINE
That inconsistency creates confusion. A pharmacist might see HYDROcodone in their EHR, but the label on the bottle from the pharmacy says Hydrocodone. A doctor orders PARoxetine, but the automated dispensing machine shows paroxetine.
That’s worse than no tall-man lettering at all. It makes people doubt the system.
In 2023, the FDA and ISMP announced they were working together to create a unified list. The first version is expected in 2024. That’s a big step forward.

How Is It Implemented?
Implementing tall-man lettering isn’t just changing fonts. It’s changing systems.
Here’s how a typical hospital does it:
- Form a team: Pharmacists, IT staff, nurses, and safety officers.
- Pick the drugs: Use ISMP or FDA lists to identify the top 50-100 most dangerous LASA pairs in your facility.
- Update systems: Apply the capitalization to your electronic health record (EHR), pharmacy software, automated dispensing cabinets (like Pyxis), and barcode scanning systems.
- Train staff: Make sure everyone knows what they’re seeing and why.
- Monitor: Track if errors go down. If not, adjust.
A 2022 study in Pharmacology Research & Perspectives followed 13 hospitals that implemented tall-man lettering across 210 drug names. It took an average of 16 weeks. The cost? Less than $1,200 per hospital in Australia. In the U.S., most of the cost is in IT labor - not software.
But here’s the catch: 68% of hospitals reported legacy systems that didn’t support tall-man lettering well. If your EHR vendor doesn’t update their system, you’re stuck.
What the Evidence Really Says
Some studies say tall-man lettering doesn’t work. A 2016 study in Pediatrics found no significant drop in errors after hospitals adopted it. But here’s the problem: researchers didn’t check if the hospitals actually implemented it correctly. Many just turned on the feature without training staff or updating all systems.
That’s like saying seatbelts don’t work because someone forgot to buckle up.
The Cochrane Collaboration reviewed all the evidence in 2022 and gave tall-man lettering a “moderate certainty” rating for reducing selection errors - but only “low certainty” for reducing actual patient harm. Why? Because it’s rarely used alone.
It’s not a magic bullet. It’s a safety net. The American Society of Health-System Pharmacists (ASHP) gives it a Grade B recommendation - meaning it’s necessary, but not enough on its own.
Dr. Michael Cohen, head of ISMP, puts it best: “Tall-man lettering is not a panacea. But it’s one essential layer in our defense-in-depth approach.”
What People on the Front Lines Say
Real-world feedback tells the real story.
Pharmacist Maria Chen in a 2023 ASHP forum said: “After we implemented ISMP’s tall-man lettering in our Epic system, we saw a 42% drop in overridden alerts for LASA drugs in six months.”
Nurse practitioner Sarah Williams wrote in the American Journal of Nursing: “The capitalized ‘SONE’ in predniSONE immediately tells me it’s not predniSOLONE. I don’t have to double-check every time.”
But not everyone is happy. Physician John Davies on Reddit complained: “I mix up ALPRAZolam and LORazepam in our EHR because the letters aren’t bold enough. The font is too small.”
And hospital pharmacist David Kim said: “Our Cerner system uses PARoxetine. Our Pyxis machine shows FLUoxetine. The community pharmacy uses different rules. It’s more confusing than helpful.”
The 2022 Wolters Kluwer survey found that 78% of pharmacists believe tall-man lettering improves safety - but 63% say it’s applied inconsistently across systems.
What’s Next for Tall-Man Lettering?
The future isn’t about replacing tall-man lettering. It’s about making it smarter.
In 2023, Epic Systems started testing an AI-powered version that adjusts capitalization based on real-time error data. If a certain drug pair keeps being confused, the system automatically makes the difference even more obvious. Early results showed a 29% greater reduction in errors than standard tall-man lettering.
Also, Australia added 12 new drug pairs to its list in March 2023 after 78 near-misses were reported. That’s how it should work - based on actual incidents, not guesswork.
Will voice recognition and barcode scanning make tall-man lettering obsolete? Maybe someday. But right now, 89% of U.S. hospitals still use it. The Joint Commission requires it. The FDA supports it. And for good reason: it works when used right.
As the Agency for Healthcare Research and Quality noted in 2023, tall-man lettering will remain a standard practice through at least 2030. Why? Because even in fully automated systems, someone still has to read the screen. And humans still make visual mistakes.
How to Use It Right
If you’re in a hospital, pharmacy, or clinic, here’s how to make tall-man lettering work for you:
- Use the ISMP list as your starting point. It’s the most comprehensive.
- Make sure all systems use the same capitalization. No exceptions.
- Train everyone - doctors, nurses, pharmacists, even students.
- Check font size. If the uppercase letters aren’t bold and clear, they’re useless.
- Monitor your error reports. If you still see mix-ups, adjust the capitalization.
- Push your EHR vendor to update. Don’t accept outdated systems.
Tall-man lettering doesn’t fix everything. But it fixes something important: the moment your eyes skip over a drug name and you almost give the wrong one.
It’s not glamorous. It doesn’t make headlines. But it saves lives - one capitalized letter at a time.
What does tall-man lettering actually do?
Tall-man lettering uses selective uppercase letters in drug names to highlight the parts that differ between look-alike, sound-alike (LASA) medications. For example, writing "predniSONE" instead of "prednisone" makes it visually distinct from "predniSOLONE," helping healthcare workers avoid mix-ups during prescribing, dispensing, or administering drugs.
Is tall-man lettering required by law?
It’s not federally mandated, but it’s required by The Joint Commission’s National Patient Safety Goal NPSG.01.01.01, which has been in place since 2004. This rule requires healthcare organizations to use methods like tall-man lettering to differentiate look-alike drug names. Most hospitals follow it to maintain accreditation.
Why do different systems show different tall-man lettering?
Different organizations - like the FDA, ISMP, and Australia’s safety commission - have their own lists of which letters to capitalize. Until a unified standard is fully adopted (expected in 2024), EHR vendors, pharmacies, and automated dispensing systems may use conflicting formats, leading to confusion for staff moving between systems.
Does tall-man lettering reduce actual patient harm?
The evidence shows it reduces selection errors - the moment a clinician picks the wrong drug from a list. However, its impact on actual patient harm is harder to prove because errors are often caught before reaching the patient. The Cochrane Collaboration rates the evidence for reducing harm as "low certainty," but still supports its use as part of a broader safety strategy.
Can tall-man lettering be used in small clinics or pharmacies?
Yes. Even small facilities can implement it using free lists from ISMP or FDA. The main challenge is getting software updates from vendors. Many pharmacy management systems and EHRs support tall-man lettering out of the box. If yours doesn’t, request it - it’s a basic safety feature, not a luxury.


Comments
Jamie Watts
Tall-man lettering is literally the bare minimum we should be doing and yet hospitals still mess it up. You think a nurse is gonna notice a capital S in predniSONE when her screen is dim and she’s on her 12th shift this week? Come on. This isn’t a fix-it’s a Band-Aid on a gunshot wound.
John Mwalwala
Let’s be real-this whole tall-man thing is just corporate theater. The real issue? Pharma companies intentionally design drug names to be confusing so they can push more scripts. It’s not about safety, it’s about profit. And don’t get me started on how EHR vendors collude with Big Pharma to keep legacy systems alive. They don’t want you to catch the error-they want you to click ‘override’ and move on. The FDA? They’re just the PR arm for the industry. Wake up.
Deepak Mishra
OMG I JUST HAD A NEAR MISS WITH HYDROmorphone AND MORPHINE!!! 😱 I thought I was safe because I saw the capitals but then my screen glitched and it showed all lowercase for 3 seconds!! I almost gave it to a kid!! 😭😭😭 We need to make ALL systems use BOLD UPPERCASE AND FLASING LIGHTS!! PLEASE!!
Rachel Wusowicz
It’s not just about the capital letters-it’s about the entire culture of rushed care. I’ve seen pharmacists skim through 80 drugs in 90 seconds while their manager yells at them to ‘hurry up.’ No amount of tall-man lettering will fix that. And the fact that some systems use ISMP and others use FDA? That’s not inconsistency-that’s negligence. They’re treating patient safety like a spreadsheet update. And it’s terrifying.
Dan Angles
While the implementation of tall-man lettering varies across systems, the underlying principle remains sound: reducing cognitive load during high-stakes decision-making is a critical component of patient safety. The evidence, when properly controlled for implementation fidelity, demonstrates a statistically significant reduction in selection errors. Institutions that treat this as a checkbox item, rather than a systemic intervention, are not failing the tool-they are failing their own protocols.
David Rooksby
Look, I get it, capital letters help-but let’s be honest, half the time the font’s so tiny you need a magnifying glass to see the difference between ‘ALPRAZ’ and ‘LOR’. And why the hell are we still using 2008-era EHRs? My hospital’s system doesn’t even support Unicode properly. I’ve seen ‘Hydrocodone’ show up as ‘Hydrocod0ne’ because some intern typed it wrong and no one fixed it. This isn’t a safety feature-it’s a gamble. And we’re all playing Russian roulette with someone else’s meds.
Melanie Taylor
As someone who works in a small clinic in rural Texas, I can say this: YES, it works! 😊 We used the ISMP list, got our vendor to update, and trained everyone-even the front desk staff. Now when a new nurse says, ‘Wait, is this predniSONE or predniSOLONE?’ I know we’re doing something right. 💪❤️ It’s not perfect, but it’s better than before. And that’s enough to keep me going.
Teresa Smith
The real tragedy isn’t that tall-man lettering isn’t perfect-it’s that we’ve accepted mediocrity as the standard. We’ve created a system where a nurse’s life-saving intuition is expected to override broken software. That’s not resilience. That’s exploitation. If we truly valued patient safety, we wouldn’t wait for a near-miss to update a font. We’d treat every capital letter as a potential life-and we’d fund the systems that make them visible.
ZAK SCHADER
Why are we wasting time on this? In America, we’ve got real problems-drugs are expensive, doctors are overworked, and now we’re fussing over CAPITAL LETTERS? This is what happens when bureaucrats run healthcare. We need more nurses, not more fonts. This is just woke safety theater. #MakeHealthcareGreatAgain