Diuretic Selector Tool
This tool helps determine the most suitable diuretic based on patient condition and clinical needs.
Reason:
Hydrochlorothiazide is a thiazide diuretic that increases urinary sodium and water loss to lower blood pressure and relieve fluid retention. It’s one of the most prescribed antihypertensive agents worldwide, with an oral half‑life of about 6‑15hours and a typical dose of 12.5‑50mg daily.
TL;DR
- Hydrochlorothiazide (HCTZ) works on the distal tubule, is cheap, and is first‑line for uncomplicated hypertension.
- Chlorthalidone offers a longer half‑life and stronger blood‑pressure control but may cause more potassium loss.
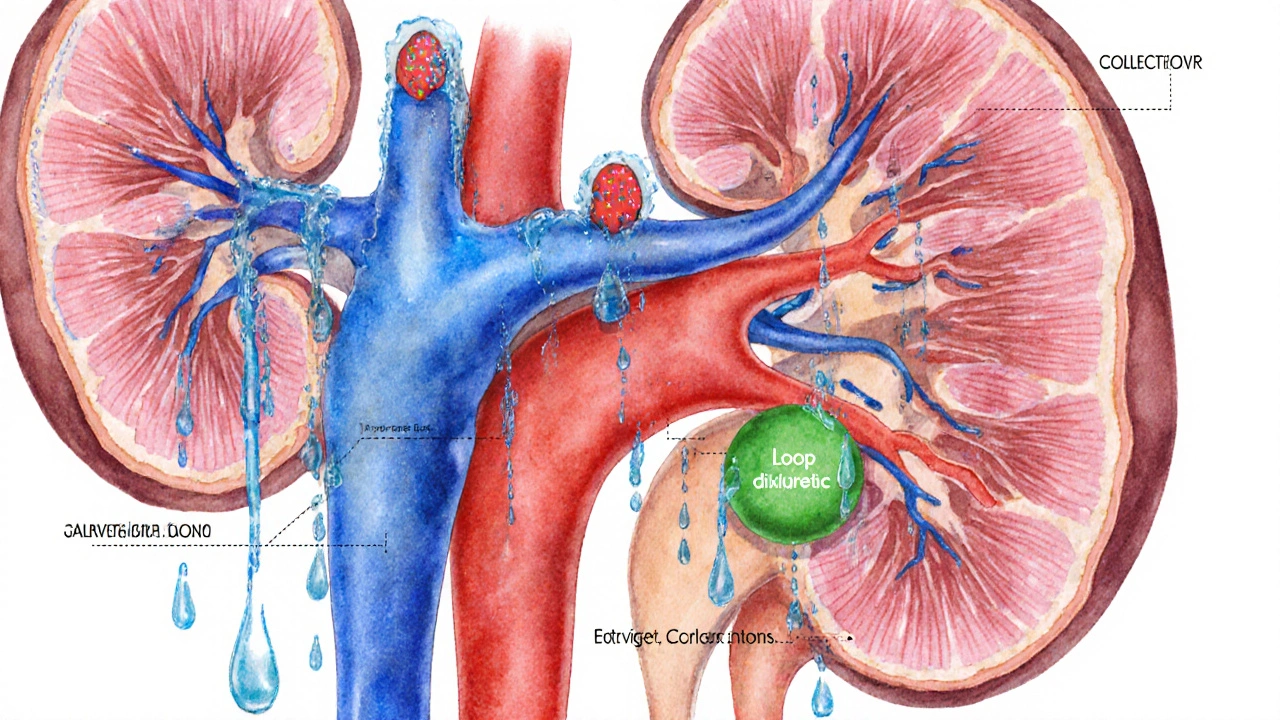
- Loop diuretics such as Furosemide act on the thick ascending limb and are best for rapid edema reduction.
- Potassium‑sparing agents like Spironolactone are useful when potassium‑saving is needed.
- Indapamide bridges the gap between thiazides and loops, offering good BP control with fewer metabolic side‑effects.
How Hydrochlorothiazide Works
The drug blocks the Na⁺/Cl⁻ cotransporter in the distal convoluted tubule. By preventing sodium reabsorption, water follows osmotically, leading to a modest‑volume depletion. The drop in plasma volume reduces cardiac output, while long‑term vascular remodeling lowers peripheral resistance.
When to Use Hydrochlorothiazide
Guidelines place HCTZ as a first‑line option for stage1‑2 hypertension without compelling comorbidities. It also manages mild‑to‑moderate peripheral edema, especially when the underlying cause is heart failure with preserved ejection fraction or chronic venous insufficiency. For severe fluid overload, clinicians usually reach for a loop diuretic first.
Safety Profile and Common Side‑Effects
Because the drug nudges electrolytes out of the body, hypokalemia, hyponatremia, and hyperuricemia are the most frequent lab abnormalities. About 5‑10% of patients report photosensitivity or mild rash. Long‑term use can mildly raise blood glucose, so diabetics need periodic monitoring.
Alternative Diuretics - Quick Overview
Below are the most common alternatives, each with a one‑sentence snapshot.
- Chlortalidone - a thiazide‑like diuretic with a 24‑hour half‑life, often more potent for blood‑pressure control.
- Furosemide - a loop diuretic acting on the thick ascending limb, ideal for rapid decongestion.
- Spironolactone - a potassium‑sparing aldosterone antagonist, useful when hypokalemia is a concern.
- Indapamide - a thiazide‑like agent with vasodilatory properties and lower metabolic disturbance.
- Metolazone - a sulfonamide diuretic that works well in combination with loops for resistant edema.
Side‑Effect Profiles of the Alternatives
Every diuretic shifts electrolytes, but the pattern differs. Loops (e.g., Furosemide) cause the biggest potassium and magnesium losses, while potassium‑sparing agents (Spironolactone) may raise potassium dangerously in kidney disease. Chlortalidone shares the same thiazide‑type metabolic changes as HCTZ but often produces a larger rise in uric acid.
Comparison Table
| Drug | Class | Primary Site of Action | Half‑Life | Typical Daily Dose | Key Side‑Effects | Best Indication |
|---|---|---|---|---|---|---|
| Hydrochlorothiazide | Thiazide | Distal convoluted tubule | 6‑15h | 12.5‑50mg | Hypokalemia, hyponatremia, hyperuricemia | Uncomplicated hypertension |
| Chlortalidone | Thiazide‑like | Distal convoluted tubule | 24h | 12.5‑25mg | Similar to HCTZ but higher potassium loss | Resistant hypertension |
| Furosemide | Loop | Thick ascending limb | 2‑3h | 20‑80mg (single dose) | Marked hypokalemia, ototoxicity at high doses | Acute pulmonary or peripheral edema |
| Spironolactone | Potassium‑sparing | Collecting duct (aldosterone antagonist) | 1.5‑2h (active metabolite 13‑15h) | 25‑100mg | Hyperkalemia, gynecomastia | Heart‑failure with reduced ejection fraction |
| Indapamide | Thiazide‑like | Distal convoluted tubule | 14‑18h | 1.5‑2.5mg | Less electrolyte disturbance, mild hypotension | Hypertension in patients prone to metabolic side‑effects |
How to Choose the Right Diuretic
Think of diuretic selection as a balancing act between efficacy, side‑effects, and patient comorbidities. Use the following quick checklist:
- Is rapid fluid removal essential? Choose a loop diuretic.
- Do you need long‑lasting blood‑pressure control with minimal dosing? Chlortalidone or Indapamide may be superior.
- Is the patient at risk for low potassium? Consider a potassium‑sparing agent or add a low‑dose potassium supplement when using HCTZ.
- Is there concurrent gout or high uric acid? Avoid thiazides if possible.
- Any known sulfonamide allergy? Skip thiazides and loops, favor Indapamide or non‑sulfonamide agents.
In practice, many clinicians start with Hydrochlorothiazide because it’s cheap, well‑studied, and works for most people with mild to moderate hypertension. If blood pressure stays high after 4‑6weeks, they either increase the dose or switch to chlortalidone before moving on to combination therapy.
Monitoring and Practical Tips
- Check serum electrolytes (Na⁺, K⁺, Mg²⁺) within two weeks of starting any diuretic.
- Re‑measure blood pressure after each dose adjustment; aim for < 130/80mmHg in most adults.
- Educate patients to report dizziness, muscle cramps, or sudden weight gain.
- If the patient develops gout flares, consider switching to a potassium‑sparing diuretic or adding allopurinol.
- Encourage a diet rich in potassium (bananas, leafy greens) when using HCTZ, unless hyperkalemia is a risk.
Related Concepts to Explore Next
Understanding diuretics connects with several broader topics. Readers often dive into:
- Renal physiology - how kidneys filter and reabsorb electrolytes.
- RAAS inhibition - why ACE inhibitors and ARBs pair well with thiazides.
- Heart‑failure management - the role of spironolactone and loop diuretics.
- Metabolic syndrome - impact of diuretics on glucose and lipid profiles.
- Gout pathophysiology - how uric acid levels rise with thiazides.
Each of these topics deepens the ability to tailor therapy to an individual’s health picture.
Frequently Asked Questions
What makes Hydrochlorothiazide a first‑line drug for hypertension?
It’s inexpensive, has a well‑defined dosing schedule, and large clinical trials have shown it reduces cardiovascular events by about 20% when used long‑term.
How does chlortalidone differ from Hydrochlorothiazide?
Chlortalidone stays in the body longer (≈24h) and delivers a steadier blood‑pressure drop, which can be advantageous in resistant hypertension. The trade‑off is a slightly higher risk of low potassium.
When should a loop diuretic be preferred over a thiazide?
Loops are the go‑to when a patient needs rapid, large‑volume fluid removal-such as in acute pulmonary edema, severe heart failure, or after major surgery.
Can I take Hydrochlorothiazide with an ACE inhibitor?
Yes, the combination is common and often more effective because the ACE inhibitor blunts the renin‑angiotensin response that thiazides can trigger.
What monitoring is required after starting a diuretic?
Check serum electrolytes and creatinine within 1‑2weeks, then repeat after any dose change. Track body weight and blood pressure weekly until stable.


Comments
April Rios
When we stare at the cascade of sodium and water that the kidneys orchestrate, we realize that each diuretic is a tiny philosopher, nudging the body toward balance. Hydrochlorothiazide, the workhorse thiazide, whispers to the distal convoluted tubule, gently coaxing sodium out of the bloodstream. This modest volume depletion translates into lower cardiac output, which over time reshapes the vasculature into a more compliant state. Yet, the elegance of HCTZ is shadowed by its metabolic side‑effects, like potassium loss and a subtle rise in uric acid that can spark gout. In contrast, chlortalidone stands as a more persistent thinker, lingering for twenty‑four hours and delivering a steadier pressure drop. The loop diuretics, such as furosemide, are the loud protestors, demanding rapid fluid removal in critical moments. Spironolactone, the potassium‑sparing sage, balances the renin‑angiotensin system while guarding against hypokalemia. Indapamide bridges the gap, offering thiazide‑like efficacy with a gentler metabolic profile. The art of choosing lies not merely in potency but in the patient’s narrative-whether they cherish a low‑cost pill or fear a flare of gout. Monitoring electrolytes becomes a ritual, a daily communion with the body’s chemistry. Lifestyle adjustments, like potassium‑rich foods, can temper the electrolyte shifts induced by HCTZ. Moreover, pairing a thiazide with an ACE inhibitor can amplify blood‑pressure control while mitigating reflex renin activation. The clinical guidelines, though evidence‑based, must be interpreted through the lens of each individual’s comorbidities. For a patient at risk of hypokalemia, a modest dose of potassium supplement or a switch to indapamide may be prudent. If the primary goal is rapid decongestion, the loop diuretic is unrivaled, albeit at the cost of greater electrolyte disturbance. Ultimately, the physician acts as the maestro, conducting these pharmacologic instruments into a harmonious symphony of blood‑pressure control and fluid balance.
byron thierry
Dear colleagues, the comparative pharmacokinetics of thiazide‑type agents underscore the clinical relevance of half‑life variability. Hydrochlorothiazide exhibits a 6‑15 hour half‑life, whereas chlortalidone extends to approximately 24 hours, offering more consistent antihypertensive coverage. It is imperative to weigh the increased potassium loss associated with longer‑acting agents against their superior efficacy in resistant hypertension. I encourage vigilant electrolyte surveillance when transitioning between these therapies.
bob zika
It is well‑documented, indeed, that the selection of a diuretic hinges upon, first and foremost, the clinical scenario, secondarily upon the patient’s metabolic profile, and, finally, upon cost considerations, which remain non‑trivial in many health‑care systems. The thiazide, Hydrochlorothiazide, provides a cost‑effective option for uncomplicated hypertension; however, the risk of hypokalemia and hyperuricemia must be addressed proactively, perhaps via supplementation or regular monitoring.
M Black
Totally agree, the cheap pills are great 👍 but don’t forget to check those labs, otherwise you’ll get caught off guard with cramps or gout flares 😂
Sidney Wachira
Behold! The humble HCTZ marches onto the stage, a knight in cheap armor, battling the tyranny of high blood pressure, yet its silent side‑kick, hyperuricemia, lurks in the shadows, ready to strike! ⚔️💊
Aditya Satria
It is essential to recognize that while thiazides are inexpensive, their impact on serum potassium and glucose can be clinically significant, especially in patients with pre‑existing metabolic disturbances. Therefore, a proactive plan-including baseline labs, scheduled follow‑up, and patient education-should be instituted before initiating therapy.
Jocelyn Hansen
Great job on laying out the comparison! 😊 Remember to tailor the choice to each patient’s comorbidities-if gout is a concern, consider indapamide; if rapid fluid removal is needed, loop diuretics are your go‑to! Keep up the thorough work! 👍
Joanne Myers
The table succinctly summarizes the key pharmacologic distinctions and aids clinicians in evidence‑based decision making.
Julie Sook-Man Chan
I prefer loops for acute edema.
Amanda Mooney
Consider patient age and renal function when selecting a diuretic; dosing adjustments may be required.
Mandie Scrivens
Oh sure, because everyone loves juggling potassium levels while counting pennies.