HP vs. Drug-Induced Lung Injury Diagnostic Tool
Symptom Assessment
Diagnostic Guidance
When you start coughing and can’t catch your breath, it’s natural to worry. Especially if you’ve recently started a new medication. Many people assume that if a drug causes lung symptoms, it must be hypersensitivity pneumonitis - the same condition linked to bird feathers, moldy hay, or humidifiers. But here’s the truth: medications do not cause true hypersensitivity pneumonitis. What they can cause is something different - and just as serious.
What Hypersensitivity Pneumonitis Really Is
Hypersensitivity pneumonitis (HP) isn’t an allergic reaction like hay fever. It’s a specific immune response in the lungs triggered by breathing in tiny particles from the environment. These aren’t drugs. They’re biological antigens - proteins from birds, fungi, bacteria, or even dust from grain or mushrooms. Think farmer’s lung from moldy hay, or bird fancier’s lung from pigeon droppings.
The body reacts by sending immune cells into the tiny air sacs of the lungs (alveoli). This causes inflammation, swelling, and sometimes the formation of small clumps of cells called granulomas. Over time, if you keep breathing in the trigger, scar tissue builds up. That’s when breathlessness becomes permanent.
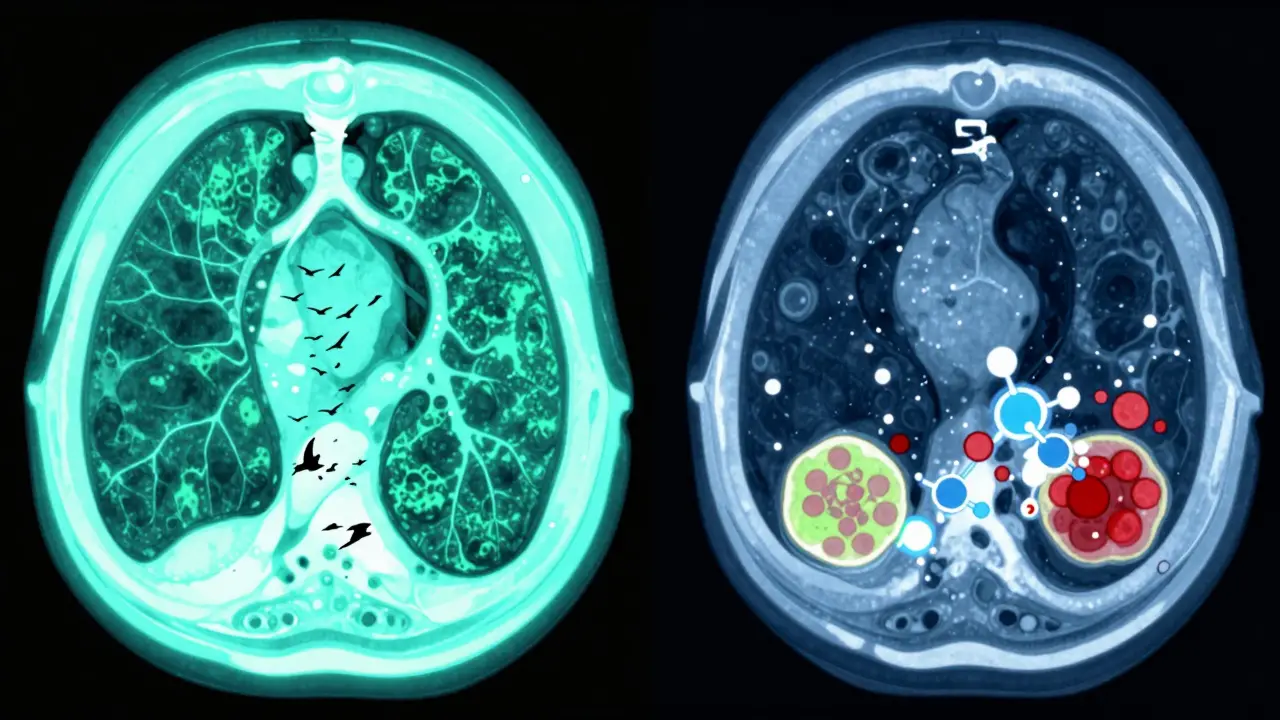
Doctors diagnose HP using a mix of clues: your history of exposure, chest scans showing ground-glass opacities or mosaic patterns, lung function tests showing reduced oxygen transfer, and sometimes a lung biopsy. The key? Symptoms get better when you’re away from the trigger - and come back when you return.
Why Medications Don’t Cause True Hypersensitivity Pneumonitis
There’s no credible evidence that pills, injections, or IV drugs cause hypersensitivity pneumonitis as defined by the Merck Manual, American Thoracic Society, or Pulmonary Fibrosis Foundation. Why? Because the mechanism is wrong.
HP requires inhalation. The antigen has to reach the deep lung through breathing. Medications enter the bloodstream. They don’t get inhaled as airborne particles. Even if a drug causes lung damage, it doesn’t trigger the same immune pattern.
True HP shows three hallmarks in lung tissue: poorly formed granulomas, lymphocytes clustering around small airways (bronchiolocentric inflammation), and a specific pattern of inflammation in the alveoli. Medication-related lung injury looks completely different. It might show organizing pneumonia, eosinophil buildup, or diffuse alveolar damage - none of which are seen in classic HP.
Major medical sources like the Merck Manual and UCSF Health list environmental triggers - not drugs - as the cause. If you search for “medication-induced hypersensitivity pneumonitis,” you won’t find it in any authoritative textbook. You’ll find it in patient forums. That’s because the terms get mixed up.
What Medications Actually Do to the Lungs
Some drugs absolutely harm the lungs. But they cause drug-induced interstitial lung disease (DILD), not hypersensitivity pneumonitis. The symptoms can feel identical: dry cough, worsening breathlessness, fatigue, even fever. But the cause and the treatment are different.
Here are real examples:
- Amiodarone (used for heart rhythm problems) - builds up in lung tissue like wax, causing inflammation and scarring. Up to 5% of long-term users develop lung damage.
- Nitrofurantoin (a common antibiotic for UTIs) - can trigger acute lung injury within days of starting. Symptoms often reverse if stopped early.
- Bleomycin (a chemotherapy drug) - causes direct toxicity to lung cells. Risk increases with cumulative dose.
- Checkpoint inhibitors (like pembrolizumab for cancer) - can cause immune-related pneumonitis, where the body attacks its own lung tissue.
These reactions don’t require repeated inhalation. They happen because the drug or its metabolites interact with lung cells directly, or because the immune system goes rogue after being activated by the drug. No mold. No bird dander. Just chemistry and biology going wrong inside the bloodstream.
How to Tell the Difference
Here’s how doctors sort it out:
- History: Did you start the drug recently? Were you cleaning a birdcage, working on a farm, or using a humidifier? Exposure history is the biggest clue.
- Imaging: High-resolution CT scans show different patterns. HP has mosaic attenuation and air trapping. Drug injury often shows patchy ground-glass or consolidation.
- Blood tests: In HP, you may have antibodies to bird proteins or mold. In drug injury, those antibodies are absent.
- Lung biopsy: The gold standard. If you see poorly formed granulomas and bronchiolocentric lymphocytes - it’s HP. If you see eosinophils or fibroblastic plugs - it’s likely a drug.
- Response to removal: If you stop the drug and symptoms improve, it’s probably DILD. If you leave the moldy barn and feel better - it’s HP.
One thing to remember: if you’re on a drug and develop cough and breathlessness, don’t assume it’s HP. But also don’t ignore it. Both conditions can become life-threatening if not caught early.
What Happens If You Keep Breathing the Trigger - or Taking the Drug
With true HP, early removal of the antigen leads to full recovery in 70-80% of acute cases. But if you keep going back to the moldy attic or the pigeon loft, fibrosis sets in. Once scar tissue forms, it doesn’t go away. Your lungs stiffen. Oxygen levels drop. You need oxygen therapy. Sometimes, a transplant.
With drug-induced injury, stopping the drug quickly can reverse damage - especially with nitrofurantoin or checkpoint inhibitors. But with amiodarone, the damage can linger for years even after stopping. The drug sticks around in fat tissue and slowly leaks out.
Chronic HP has a 5-year survival rate of 50-80%. Drug-induced fibrosis? Survival depends on the drug and how fast you act. Bleomycin damage is often irreversible. Amiodarone fibrosis progresses slowly but steadily.

What Should You Do If You Have Cough and Breathlessness?
Don’t panic. But don’t wait.
- Write down everything: When did symptoms start? What changed in your life? New pet? New job? New medication? Cleaning the basement? Using a new humidifier?
- Don’t stop your meds on your own. Talk to your doctor. Some drugs can’t be stopped suddenly.
- Ask for a chest CT scan. It’s the most important test.
- Request pulmonary function testing - especially DLCO (diffusing capacity). A drop here is a red flag.
- Ask if you should see a pulmonologist who specializes in interstitial lung disease. Not all lung doctors know the difference between HP and DILD.
Many patients spend months going in circles because their doctor assumes it’s asthma or bronchitis. If your cough doesn’t respond to inhalers, and your breathlessness gets worse with activity, push for deeper investigation.
Bottom Line
Hypersensitivity pneumonitis is not caused by pills. It’s caused by what you breathe. If you have cough and breathlessness after starting a new medication, you may have drug-induced lung injury - not HP. But both need urgent attention.
The good news? If caught early, both can be managed. The bad news? If ignored, both can lead to permanent scarring. Don’t let confusion delay your diagnosis. Know the difference. Ask the right questions. And don’t assume a label just because it sounds familiar.
Can medications cause hypersensitivity pneumonitis?
No. True hypersensitivity pneumonitis is caused by inhaling environmental antigens like mold, bird proteins, or bacteria. Medications enter the bloodstream and cause different types of lung injury, such as drug-induced interstitial lung disease (DILD), which has distinct causes, symptoms, and pathology. Medical authorities like the Merck Manual and American Thoracic Society do not list medications as causes of true HP.
What are the most common drugs that cause lung damage?
Common culprits include amiodarone (for heart rhythm), nitrofurantoin (for urinary infections), bleomycin (a chemotherapy drug), and immune checkpoint inhibitors like pembrolizumab. These drugs can cause inflammation, scarring, or direct toxicity to lung tissue, but they do not trigger the granulomatous, inhalation-based immune response seen in hypersensitivity pneumonitis.
How do I know if my cough is from a drug or from mold/bird exposure?
Look at timing and context. If your cough improves when you’re away from your home or workplace - like on vacation - and returns when you come back, it’s likely environmental. If your cough started after beginning a new medication and doesn’t change with location, it’s more likely drug-related. A high-resolution CT scan and lung biopsy can confirm the pattern of damage.
Is hypersensitivity pneumonitis curable?
In acute cases, yes - if you remove the trigger early. Most people recover fully within weeks. In chronic cases, especially with scarring (fibrosis), it’s not curable but can be managed. Treatments include corticosteroids, immunosuppressants, and antifibrotic drugs like nintedanib. The goal is to slow progression and preserve lung function.
Should I stop my medication if I develop a cough?
Never stop a prescribed medication without talking to your doctor. Some drugs, like heart or seizure medications, can be dangerous to stop abruptly. Instead, contact your doctor immediately. They may order tests like a chest CT or lung function test to determine the cause. Stopping a drug too soon without confirmation can delay diagnosis and worsen outcomes.


Comments
Janette Martens
i just read this and thought my cough from my new heart med was hp cause i clean my parrot’s cage every week… turns out i was wrong but still scared as hell. thanks for clarifying. i’m gonna call my doc monday.
Marie-Pierre Gonzalez
Thank you for this meticulously researched and profoundly important clarification. It is imperative that the medical community and the public alike distinguish between environmental hypersensitivity pneumonitis and drug-induced interstitial lung disease. Mislabeling can lead to inappropriate management, delayed diagnosis, and unnecessary psychological distress. I urge all healthcare providers to adopt precise terminology and educate their patients accordingly. With profound respect, I remain,
Marie-Pierre Gonzalez, R.N., B.Sc.N., C.C.N.
Louis Paré
So let me get this straight - you’re telling me people are panicking over a word? ‘Hypersensitivity pneumonitis’ sounds fancy so they slap it on everything. Meanwhile, real medicine is over here with CT scans and biopsy results and nobody’s reading the Merck Manual anymore because TikTok told them their amiodarone is ‘making their lungs cry.’ Pathetic. This post is the only thing keeping me from moving to Antarctica.
Hakim Bachiri
Okay but… who even defines what ‘true’ HP is? The American Thoracic Society? Who elected them? Meanwhile, in Japan, they classify some drug reactions under HP-like categories because the immune response looks similar on histology. And don’t even get me started on the WHO’s 2023 revision… I’ve seen papers that argue the distinction is arbitrary. This isn’t science - it’s semantics dressed up as authority. Also, amiodarone is basically liquid lava. Everyone knows that.
Celia McTighe
Thank you so much for writing this ❤️ I’ve been having this cough for 3 months and my doctor kept saying ‘it’s just allergies’… I finally pushed for a CT and it showed ground-glass opacities. They thought it was HP because I got a new parrot. But I’d been on nitrofurantoin for 6 weeks. We stopped it and my lungs are already improving. I feel seen. Also, if anyone else is scared - you’re not alone. I cried reading this. You’re doing great.
Ryan Touhill
Interesting. But have you considered that the real agenda here is pharmaceutical industry influence? The ATS and Merck Manual are funded by Big Pharma. They don’t want you to know that drugs like checkpoint inhibitors cause HP-like reactions because then lawsuits would skyrocket. They reclassify everything as ‘DILD’ to avoid liability. I’ve seen patients with identical pathology - one labeled HP, the other DILD - just because one had a bird and the other had a prescription. Coincidence? I think not. Also, your humidifier comment? That’s a distraction. The real trigger is glyphosate in the water.
ANA MARIE VALENZUELA
Wow. Just… wow. You’re telling me people are misdiagnosing themselves based on Google and then blaming their doctors? And you’re surprised? This is why we can’t have nice things. You wrote a 2000-word essay and still didn’t mention that 40% of ‘drug-induced’ cases are actually undiagnosed HP because the patient lied about their bird exposure. Don’t give me this ‘meds don’t cause HP’ nonsense - I’ve seen the slides. It’s not black and white. Stop being so dogmatic.
Bradly Draper
so if i stop the medicine and feel better, it's probably the medicine? and if i go on vacation and feel better, it's the bird stuff? that's all i need to know. thanks.
Samantha Hobbs
wait so i was right to be mad at my husband for bringing home that used birdcage?? i told him it was gonna make me sick and he said i was being dramatic. now i have a cough and he’s acting like it’s all in my head. also i think my doctor is an idiot. can i just sue someone??