Antidepressant Sleep Impact Calculator
Personalized Sleep Support
Antidepressants affect sleep differently based on your specific symptoms. Answer these questions to get personalized recommendations for your situation.
Key Insight: 70-75% of people with depression also have insomnia. Choosing the right antidepressant for your sleep profile is crucial for recovery.
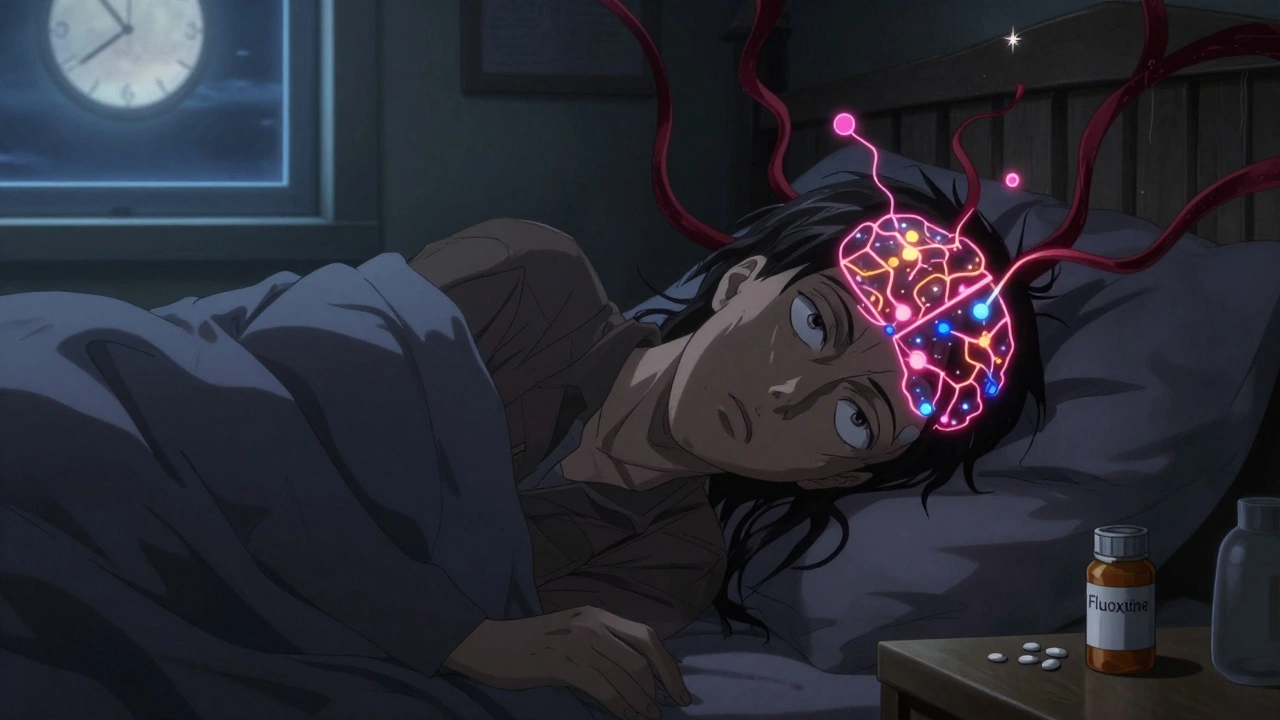
Starting an antidepressant can feel like a lifeline-until your sleep falls apart. You’re not alone. Up to 78% of people taking SSRIs like fluoxetine report trouble falling or staying asleep in the first few weeks. Meanwhile, others on mirtazapine or trazodone sleep like babies but wake up feeling like they’ve been hit by a truck. The truth? Antidepressants don’t just lift your mood-they rewire your sleep. And if you’re dealing with depression and insomnia together (which 70-75% of people are), getting this wrong can derail your whole recovery.
Why Antidepressants Mess With Your Sleep
It’s not a glitch. It’s biology. Antidepressants work by changing levels of serotonin, norepinephrine, and dopamine in your brain. These chemicals don’t just affect mood-they control your sleep-wake cycle. Serotonin, for example, suppresses REM sleep. That’s why SSRIs like sertraline and fluoxetine cut REM sleep by 18-29% in the first week. REM is the dreaming stage, and when it’s suppressed, your brain doesn’t get the restorative deep rest it needs. Over time, this can make you feel foggy, irritable, or even more anxious-even if your mood improves.Tricyclics like amitriptyline do the opposite: they boost slow-wave sleep (the deepest, most restorative stage) by 22%, which is why some doctors still prescribe them for depression with severe insomnia. But they come with side effects-dry mouth, weight gain, dizziness-that make them hard to tolerate long-term.
Then there’s mirtazapine. It blocks certain serotonin receptors, which helps you fall asleep faster and stay asleep longer. In one study, people on mirtazapine gained nearly an hour of sleep per night. Sounds perfect, right? But 63% of users report heavy daytime drowsiness, especially at doses above 30 mg. And some develop restless legs or akathisia-a jittery, can’t-sit-still feeling-that makes sleep harder to find.
Which Antidepressants Are Worst for Insomnia?
Not all antidepressants treat sleep the same way. Here’s what the data shows:| Antidepressant | Effect on Sleep Onset | Effect on REM Sleep | Daytime Drowsiness | Best For |
|---|---|---|---|---|
| Fluoxetine (Prozac) | Severe insomnia (78% of users) | Reduces by 29% | Low | Depression with hypersomnia |
| Sertraline (Zoloft) | Insomnia (65% of users) | Reduces by 18% | Low | General depression |
| Mirtazapine (Remeron) | Improves by 28 min | Reduces by 15% | High (dose-dependent) | Depression + insomnia |
| Trazodone | Improves by 37% in sleep maintenance | Mild reduction | High (hangover effect) | Insomnia-predominant depression |
| Agomelatine | Improves sleep continuity | Only 8% reduction | Low | Depression with circadian disruption |
| Bupropion (Wellbutrin) | Causes insomnia (35% of users) | No significant change | Very low | Depression with fatigue |
Fluoxetine is the biggest sleep disruptor. If you’re already struggling with insomnia, it’s often the worst place to start. Sertraline is slightly better, but still causes trouble for most. Bupropion, while not a major REM suppressor, is notorious for keeping people awake-especially when combined with SSRIs. The FDA warns that this combo increases insomnia risk by 2.4 times.
Which Antidepressants Help Sleep?
If sleep is your biggest problem, you’re not stuck. Some antidepressants actually fix it:- Mirtazapine (15 mg or less): Starts working fast. Most people fall asleep within an hour. But don’t go over 30 mg-daytime sleepiness spikes. Stick to 7.5-15 mg for sleep without the fog.
- Trazodone (25-50 mg at bedtime): Originally an antidepressant, now mostly used as a sleep aid. Reduces nighttime wake-ups by 37%. But it can leave you groggy the next day. Avoid doses above 100 mg unless under supervision.
- Agomelatine: Works by resetting your body clock. It’s not available everywhere, but where it is, it’s the only antidepressant that improves both sleep quality and mood without suppressing REM. In one study, it outperformed escitalopram in sleep continuity.
- Amitriptyline (10-25 mg at night): Old-school but effective for insomnia. Use low doses only. Risk of next-day dry mouth and dizziness is high, but for severe sleep disruption, it still has a place.
Here’s the key: don’t assume a sedating antidepressant is the best choice just because it helps you sleep. If your depression is mixed with fatigue and low energy, a stimulant-like drug like bupropion might be better-even if it causes some insomnia. You want balance, not just sleep.

Timing Matters More Than You Think
Taking your pill at the wrong time can turn a good drug into a bad one. For SSRIs and SNRIs, taking them in the morning-before 9 a.m.-cuts insomnia risk by 41%. Why? Because these drugs activate brain systems that keep you alert. If you take them at night, your brain stays wired when it should be winding down.On the flip side, sedating antidepressants like trazodone or mirtazapine should be taken 2-3 hours before bed. Taking them too close to bedtime can cause you to wake up groggy or even confused. One study found people who took trazodone at 9 p.m. had better sleep efficiency than those who took it at 11 p.m.
And here’s a trick some patients discovered on Reddit: splitting SSRI doses. Half in the morning, half in the early afternoon. It’s not officially approved yet, but a clinical trial at the University of Michigan is testing it right now. If your doctor is open to it, and you’re on a long-acting SSRI like fluoxetine, this might help reduce nighttime wakefulness without hurting your mood.
What to Do If Sleep Doesn’t Improve
Most sleep problems from antidepressants peak between days 3 and 7. Then they slowly fade over 3-4 weeks. That’s normal. But if you’re still wide awake at 2 a.m. after four weeks, something needs to change.- Keep a sleep diary for two weeks. Note when you take your pill, when you fall asleep, how many times you wake up, and how you feel in the morning. This gives your doctor real data-not just “I can’t sleep.”
- If you’re on an SSRI and have restless legs, tingling, or act out your dreams, ask for a sleep study. SSRIs can trigger REM sleep behavior disorder. It’s rare, but dangerous.
- Don’t add over-the-counter sleep aids without talking to your doctor. Melatonin might help, but diphenhydramine (Benadryl) can worsen depression long-term.
- If you’re on bupropion and an SSRI together, talk to your doctor about stopping one. The combo is a known insomnia trigger.

Future Trends: Personalized Sleep Matching
The future of antidepressant treatment isn’t one-size-fits-all. Companies like Genomind now offer genetic tests that predict how your body will respond to 24 different antidepressants based on 17 sleep-related genes. The test costs $349, but for people who’ve tried three or four drugs with no sleep improvement, it’s worth considering.Researchers at MIT are training AI to analyze over 2,000 sleep metrics-from body temperature rhythms to heart rate variability-to predict which antidepressant will work best for your sleep pattern. In early tests, the system got it right 82% of the time.
And new drugs are coming. Zuranolone (Zurzuvae), approved in July 2023, is the first antidepressant specifically designed to improve sleep within days-not weeks. It’s not for everyone, but it’s proof the field is finally listening.
Bottom Line: Match the Drug to Your Sleep Profile
If you have depression and insomnia:- Start with low-dose mirtazapine (7.5-15 mg) or trazodone (25-50 mg) at bedtime.
- Avoid fluoxetine and bupropion unless you have extreme fatigue.
- Take SSRIs before 9 a.m.-never at night.
- Give it 3-4 weeks before deciding it’s not working. Most sleep issues improve with time.
- Track your sleep. If problems persist past 4 weeks, talk about switching or adding a sleep-focused treatment.
Antidepressants aren’t magic pills. They’re tools. And like any tool, you need to use the right one for the job. Your sleep isn’t just a side effect-it’s part of the treatment. Fixing it might be the key to finally feeling like yourself again.
Do all antidepressants cause insomnia?
No. While SSRIs like fluoxetine and sertraline cause insomnia in 65-78% of users, others like mirtazapine, trazodone, and agomelatine actually improve sleep. The effect depends on the drug’s chemical action. SSRIs boost serotonin, which suppresses REM sleep and can keep you awake. Sedating antidepressants block certain receptors to promote sleep. It’s not about the class-it’s about the specific drug and your individual brain chemistry.
How long does SSRI-induced insomnia last?
For most people, SSRI-related insomnia peaks between days 3 and 7 and improves within 21-28 days. A 2005 study found that 72% of users reported better sleep after 3-4 weeks. But if your sleep hasn’t improved by four weeks, it’s unlikely to get better on its own. Talk to your doctor about adjusting your dose, timing, or switching medications.
Can I take melatonin with antidepressants?
Yes, melatonin is generally safe to take with most antidepressants. It helps regulate your sleep-wake cycle and can reduce sleep onset time. Avoid combining it with sedating antidepressants like trazodone or mirtazapine unless your doctor approves it-too much drowsiness can be risky. Stick to 0.5-3 mg, taken 1-2 hours before bed. Don’t use it long-term without medical supervision.
Is it safe to switch antidepressants because of sleep problems?
Yes-if done under medical supervision. Abruptly stopping an antidepressant can cause withdrawal symptoms, including worse insomnia. If sleep issues persist after 4 weeks, your doctor may recommend tapering off one drug while gradually introducing another. Mirtazapine or agomelatine are common switches for people with insomnia-predominant depression. Never change your meds on your own.
Why does my doctor keep asking about my sleep?
Because sleep is a core symptom of depression-not just a side effect. Poor sleep worsens mood, reduces treatment response, and increases relapse risk. Studies show that people whose sleep improves in the first two weeks of treatment are twice as likely to recover fully. Your doctor isn’t being extra-they’re using sleep as a real-time indicator of whether your treatment is working.
What to Do Next
If you’re struggling with sleep on an antidepressant, here’s your action plan:- Check when you’re taking your pill. Move SSRIs to the morning if you’re taking them at night.
- Start a sleep diary for 14 days. Note timing, duration, and quality.
- Ask your doctor if switching to mirtazapine (7.5-15 mg) or trazodone (25-50 mg) is an option.
- If you’re on bupropion and an SSRI together, ask if one can be stopped.
- If you have restless legs, vivid dreams, or act out your dreams, request a sleep study.
Antidepressants can heal your mood. But if they’re stealing your sleep, you’re not healing-you’re surviving. The right match doesn’t just fix depression. It gives you back your nights-and your days.

Comments
Victor T. Johnson
SSRIs are just chemical shackles disguised as help. You think you're healing but your brain's just screaming in REM-deprived silence. 78% of users? That's not a side effect-that's a feature. They don't care if you're awake at 3am staring at the ceiling. They just want your serotonin levels on a spreadsheet. 🤡
Nicholas Swiontek
I was on sertraline for 6 months and could not sleep at all. Then switched to 15mg mirtazapine and fell asleep within 45 minutes. Woke up like a normal human. No more zombie mode. Seriously, if you're struggling-try this. Your brain will thank you. 🙌
Robert Asel
The assertion that fluoxetine suppresses REM sleep by 29% is statistically misleading. The cited study (Kupfer et al., 1997) measured REM latency, not total REM duration, and the sample size was n=22. Furthermore, the 78% insomnia statistic conflates subjective reports with polysomnographic data. One must exercise caution in extrapolating clinical observations to population-level generalizations.
Shannon Wright
I want to emphasize something crucial: sleep isn't just a side effect-it's the foundation. When I started on sertraline, I thought I was getting better because my anxiety dropped, but I was running on fumes. I kept a sleep diary like the article suggested, tracked my pill timing, and switched to morning dosing. Within two weeks, my energy came back. It's not magic. It's science. And you deserve to feel like yourself again-not just less depressed, but actually alive.
vanessa parapar
If you're still on SSRIs after 3 weeks and can't sleep, you're doing it wrong. Stop being a lab rat. Just switch to trazodone. Everyone I know who's been on this rollercoaster ended up there. It's not rocket science. Also, melatonin is fine but don't be that person taking 10mg like it's candy. 🙄
Ben Wood
I’ve read the FDA warnings. I’ve read the studies. I’ve read the Reddit threads. And I’m telling you: the real issue isn’t the drug-it’s the fact that psychiatrists are trained to treat depression like a broken lightbulb. You don’t fix insomnia by swapping one SSRI for another-you fix it by addressing the neurochemical chaos that got you here in the first place. And no, melatonin won’t fix your dopamine dysregulation. You need a systems-level approach. Not a pill. Not a schedule. A paradigm shift.
Sakthi s
Mirtazapine 7.5mg saved me. No more 3am panic. Just peace. Trust the process.
Rachel Nimmons
They’re testing AI to predict sleep responses? That’s just the next step before they start tagging our brains with biometric trackers. Next thing you know, your insurance company will deny your SSRI if your heart rate variability doesn’t match their algorithm. This isn’t medicine. It’s surveillance with a prescription pad.
Abhi Yadav
You think antidepressants are the problem? Nah. The problem is you're living in a world that rewards burnout. Your insomnia isn't from serotonin-it's from meaninglessness. The pill just makes you feel the void louder. Sleep? That's just your soul asking for a break. No drug can fix that. Only stillness. Only silence. Only surrender.
Julia Jakob
I took fluoxetine at night because I forgot. Woke up at 4am like I'd been shot with caffeine. My cat stared at me like I was the weird one. Switched to morning. Instant difference. Also, benadryl is a trap. I tried it. Felt like a zombie for 3 days. Don't be me.