When you’re on Medicaid, getting your prescriptions shouldn’t mean choosing between medicine and rent. But knowing what’s covered - and what’s not - can feel like navigating a maze. In 2025, Medicaid covers outpatient prescription drugs for nearly 85 million low-income Americans, but the details vary wildly by state. Some states make it easy. Others make you jump through hoops. Here’s what you actually need to know.
Medicaid Covers Prescriptions - But Not All of Them
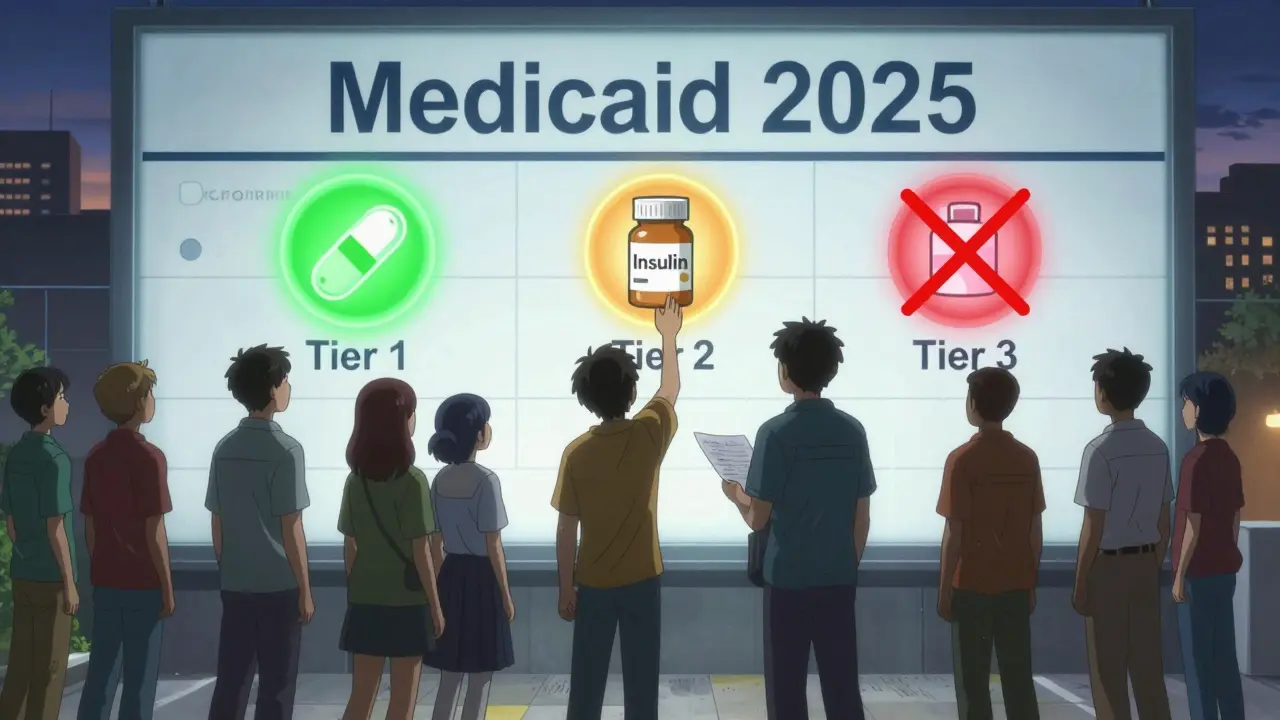
Federal law doesn’t require Medicaid to pay for prescription drugs, but every single state does. That’s because covering medications saves money in the long run. A person with diabetes who can’t afford insulin ends up in the ER. A person with high blood pressure who skips pills risks a stroke. Medicaid knows this. So it pays for meds - mostly. But not every drug is on the list. Each state creates its own Preferred Drug List (PDL), which sorts medications into tiers. Tier 1 is usually generic drugs with the lowest copay. Tier 2 is brand-name drugs with higher costs. Tier 3? That’s often specialty drugs - expensive ones for conditions like rheumatoid arthritis or hepatitis C. For example, in North Carolina, a generic blood pressure pill might cost $3. A brand-name version? $25. And a specialty drug for multiple sclerosis? You could pay $100 or more - unless you qualify for extra help.Step Therapy: You Have to Fail First
One of the biggest surprises for new Medicaid beneficiaries? You might not get the drug your doctor prescribed right away. Many states require step therapy - also called "trial and failure." Here’s how it works: Your doctor prescribes Drug A. But Medicaid’s formulary says Drug B is preferred. So you have to try Drug B first. If it doesn’t work - or causes side effects - you try Drug C. Only after failing two preferred drugs can you get Drug A. And yes, that’s legal. North Carolina requires this for most chronic conditions. Florida does too. So do 38 other states. The idea? Save money by pushing cheaper, proven drugs first. But the reality? People wait. Sometimes for weeks. A 2024 survey by the Medicare Rights Center found that 63% of Medicaid beneficiaries faced delays because of step therapy. One Reddit user in North Carolina wrote: "I had to try three SSRIs before they’d approve Wellbutrin. My depression got worse. I missed work. I cried every day waiting for approval."Prior Authorization: Paperwork That Can Delay Care
Even if a drug is on the formulary, you might still need prior authorization. That means your doctor has to submit paperwork - often including lab results, diagnosis codes, and proof you tried other drugs - before Medicaid will pay. Some drugs require it every time. Others only once, for up to three years. In North Carolina, people with Type 1 Diabetes using premixed insulin can get a prior authorization that lasts three years. But if you switch to a different insulin, you start over. The process isn’t fast. The average approval takes 7.2 business days. If it’s denied? You appeal. That takes another 14.5 days on average. But here’s the good news: 78% of denials get overturned when your doctor submits full clinical notes. Don’t give up. Push back. Ask your doctor to write a detailed letter explaining why the preferred drug won’t work for you.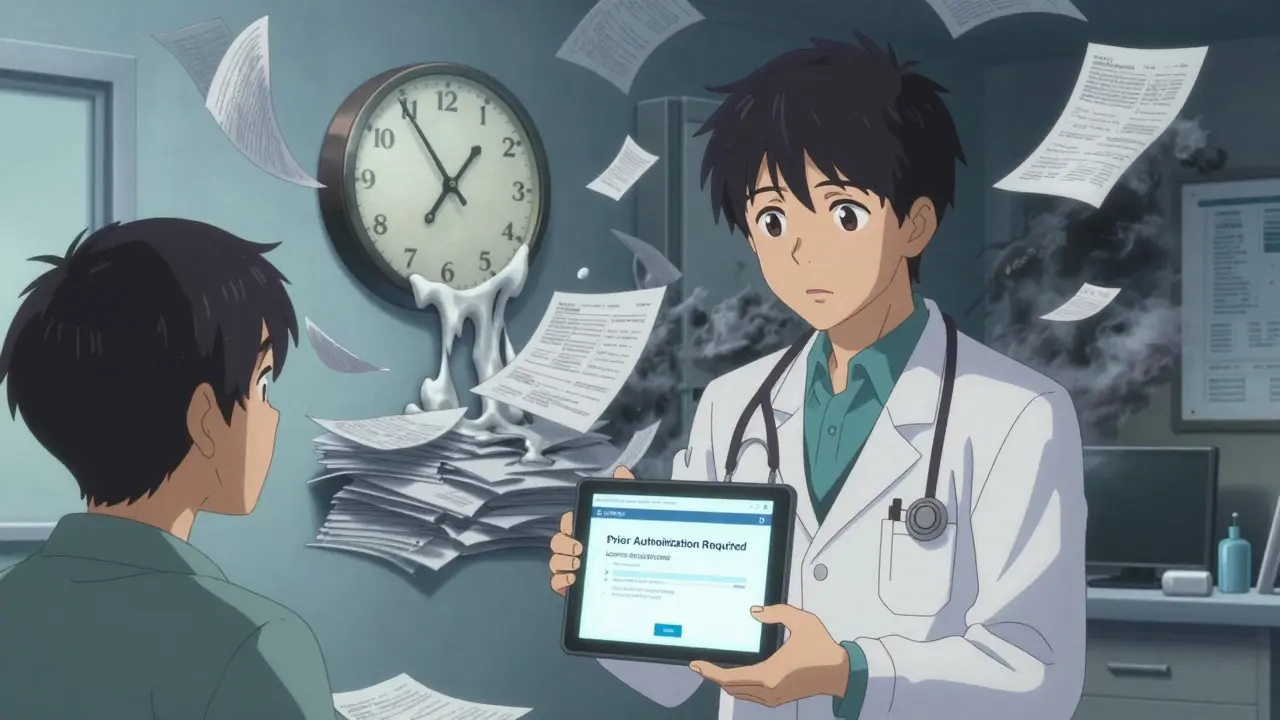
Costs: Copays, Deductibles, and the Extra Help Program
Medicaid doesn’t charge premiums for most enrollees. But copays? They exist - and they vary. - Generics: Usually $1-$5 - Brand-name drugs: $5-$25 - Specialty drugs: $50-$150, sometimes more But if you qualify for Extra Help (also called the Low-Income Subsidy), your costs drop dramatically. In 2025: - $0 monthly premium - $0 deductible - $4.90 copay for generics - $12.15 for brand-name drugs - After you spend $2,000 total on drugs in a year? You pay $0 for everything else. Here’s the catch: If you have full Medicaid coverage, you automatically qualify for Extra Help. But 1.2 million people who are eligible don’t know it. Check with your state Medicaid office or call 1-800-MEDICARE. Don’t assume you’re not eligible.What’s Not Covered? The Hidden Gaps
Not every drug makes the list. States remove medications all the time - usually because they no longer offer rebates or cost too much. In North Carolina’s October 2025 formulary update, these drugs were dropped: - Vasotec Tablet - Acanya Cream - Trulance Tablet - Vanos Cream - Solodyn ER Tablet - Apriso Capsule Some were removed because manufacturers stopped offering rebates. Others? They were replaced with cheaper alternatives. If your drug disappeared from the formulary, your doctor can request an exception - but it’s not guaranteed. Also, over-the-counter drugs? Generally not covered. Unless you have a prescription for them. And even then, it’s rare.Network Pharmacies and Mail Order
You can’t just walk into any pharmacy. Medicaid works with specific network pharmacies. CVS, Walgreens, Rite Aid - most are in. But small local pharmacies? Not always. For maintenance meds (like blood pressure or diabetes pills), many states push you toward mail-order services. You get a 90-day supply shipped to your house - often at a lower cost. But if you’re not comfortable with mail order, you can usually still use a local pharmacy. Just confirm they’re in-network first.
How to Find Your State’s Formulary
There’s no national Medicaid formulary. You need your state’s. Here’s how: 1. Go to your state’s Medicaid website (search "[Your State] Medicaid formulary") 2. Look for "Preferred Drug List" or "PDL" 3. Download the PDF - it’s usually updated every 3-6 months 4. Search your drug by name or generic ingredient 5. Check the tier and any restrictions (step therapy, prior auth) If you’re stuck, call your state’s Medicaid helpline. Or find a local SHIP counselor (State Health Insurance Assistance Program). They help people navigate this stuff every day.What’s Changing in 2025-2026?
New rules are coming. In September 2025, CMS announced it will require states to prove their formularies don’t block access to medically necessary drugs. That’s a big shift. For years, states could restrict drugs without showing harm. Now, they’ll have to justify it. Also, the Inflation Reduction Act’s $2,000 out-of-pocket cap for Medicare Part D now applies to dual-eligible beneficiaries (those on both Medicare and Medicaid). That means if you’re on both programs, your drug costs are capped - even if your state’s Medicaid formulary is strict. And experts predict more gene therapies will hit the market by 2027 - each costing over $2 million. Medicaid programs are already testing new payment models to handle these drugs without bankrupting budgets.What to Do Right Now
If you’re on Medicaid and take prescriptions: - Know your state’s formulary. Check it every six months - they change often. - Ask your doctor: "Is this drug on the PDL? Do I need prior auth?" - If your drug was removed or denied, ask for a formulary exception. Bring your doctor’s note. - If you’re paying more than $5 for generics or $25 for brands, ask if you qualify for Extra Help. - Use mail-order for maintenance meds to save money and time. - Keep copies of all prior auth approvals and denials. Medicaid isn’t perfect. But it’s the biggest safety net we have for low-income Americans needing prescriptions. Understanding how it works - the tiers, the steps, the paperwork - means you’re not just a patient. You’re an advocate.Does Medicaid cover all prescription drugs?
No. Medicaid covers most outpatient prescription drugs, but each state creates its own Preferred Drug List (PDL). Some drugs are excluded because they don’t offer rebates, are too expensive, or have cheaper alternatives. Always check your state’s current formulary before assuming a drug is covered.
What is step therapy in Medicaid?
Step therapy means you must try and fail on one or two lower-cost, preferred drugs before Medicaid will cover the one your doctor prescribed. For example, if your doctor prescribes a brand-name antidepressant, you may first need to try two generic options. This rule exists in 38 states and can cause delays in treatment.
How do I get prior authorization for a drug?
Your doctor must submit paperwork to your state’s Medicaid program or pharmacy benefit manager (PBM). This usually includes your diagnosis, why preferred drugs won’t work, and sometimes lab results. The process takes 7-14 days. If denied, appeal with more clinical documentation - 78% of appeals are approved when complete.
Can I use any pharmacy with Medicaid?
No. You must use a pharmacy in your state’s Medicaid network. Most major chains like CVS and Walgreens are included, but smaller pharmacies may not be. Always confirm before filling a prescription. For long-term medications, mail-order services often offer lower copays and 90-day supplies.
What is Extra Help, and do I qualify?
Extra Help (Low-Income Subsidy) is a federal program that lowers prescription costs for people with limited income. If you have full Medicaid coverage, you automatically qualify. Benefits include $0 premiums, $0 deductibles, $4.90 copays for generics, and $12.15 for brand-name drugs. After spending $2,000 in a year, you pay nothing. About 1.2 million eligible people don’t know they qualify - check with Medicaid or call 1-800-MEDICARE.
Why do Medicaid formularies change so often?
Formularies change because drug prices shift, rebates expire, and new generics enter the market. States update lists to save money - often removing drugs that no longer offer financial rebates from manufacturers. North Carolina, for example, removed 12 drugs in 2025 because they were no longer rebate-eligible. Always check your formulary every 6 months.
Are over-the-counter drugs covered by Medicaid?
Generally, no. Medicaid doesn’t cover OTC drugs unless they’re prescribed by a doctor and meet specific medical criteria - which is rare. Even then, coverage varies by state. Always ask your pharmacist or Medicaid office before assuming an OTC drug is covered.

Comments
Katie Taylor
Look, I’ve been on Medicaid for 7 years and this article is spot-on. I had to fight for 3 months to get my antidepressant approved after they made me try 4 generics that made me feel like a zombie. I called my state’s helpline, printed out my doctor’s note, and sent it certified mail. Got approved in 11 days. Don’t let bureaucracy break you - fight back. You’re not asking for luxury, you’re asking to survive.
And yes, Extra Help is automatic if you have full Medicaid. Stop assuming you don’t qualify. Call 1-800-MEDICARE right now. It’s free. Your insulin shouldn’t cost more than your rent.
Sidra Khan
So Medicaid covers drugs but only if they’re cheap enough? Fascinating. Next they’ll tell me oxygen is covered only if I breathe through a straw. 🤡
Step therapy? Sounds like they’re running a clinical trial on my body. Why not just let the doctor decide? Oh right - because profit > people. Classic.
Ademola Madehin
Bro. I had to wait 47 days for my MS med. 47. DAYS. I was in a wheelchair. My wife cried. My cat stopped purring when I walked in the room. I had to beg my doctor to write a letter. Then they denied it. Then I screamed into a pillow for 2 hours. Then I emailed my senator. Then I got it.
Medicaid ain’t a program. It’s a trauma simulator. And y’all act like it’s normal? It’s not. It’s torture with paperwork.
suhani mathur
For those asking how to check your formulary: Go to your state’s Medicaid site. Type ‘Preferred Drug List’ into the search bar. If you get nothing, call them. If they put you on hold for 40 minutes, hang up and call back at 8:03 AM - they’re less busy then.
And if your drug got removed? Ask for a ‘formulary exception’ - not a ‘special request.’ Use the exact phrase. It matters. I’ve helped 3 people get their meds back just by knowing the right words.
Also - mail order saves you time and money. I get 90 days of metformin delivered to my door for $2. No lines. No stress. Do it.
bharath vinay
They say Medicaid covers meds to save money. But let’s be real - this is all a cover for Big Pharma and the government to control what drugs you can take. You think they care if you live? No. They care if you stay quiet. That’s why they make you jump through hoops. Step therapy? Prior auth? It’s psychological warfare. They want you to give up. Don’t. Fight. They’re scared of people who know their rights.
And why is Extra Help automatic? Because they don’t want you to know how much you’re owed. They want you to think you’re lucky to get anything at all. Wake up.
Wilton Holliday
Hey - if you’re reading this and you’re stressed about your meds, I see you. You’re not alone.
Here’s what worked for me: I printed out my state’s formulary, highlighted every drug I take, and took it to my doctor’s next appointment. I said: ‘I need to know if any of these are at risk.’ She looked at it, said ‘oh wow, this one’s being pulled next month,’ and started the exception paperwork right then.
Also - if you’re paying more than $5 for a generic, you’re probably not getting Extra Help. Call 1-800-MEDICARE. It takes 5 minutes. You’ll thank yourself later.
You’re not a burden. You’re a patient. And you deserve care.
Joseph Manuel
The article contains a number of factual inaccuracies and misleading generalizations. For instance, the assertion that ‘78% of denials are overturned upon appeal’ is drawn from a non-peer-reviewed survey with an unverified sample size. Furthermore, the claim that Medicaid ‘automatically’ qualifies beneficiaries for Extra Help is only true for those enrolled in full-scope Medicaid; those in expanded or limited-benefit programs may not qualify. Additionally, the term ‘step therapy’ is mischaracterized as a punitive measure, when in fact it is an evidence-based utilization management tool endorsed by the American College of Physicians. The tone of this piece is alarmist and lacks nuance, which risks undermining informed public discourse on sustainable healthcare policy.
Harsh Khandelwal
They got rid of Vasotec? LMAO. That’s the drug my uncle used before he died of kidney failure. They replaced it with some ‘generic alternative’ that made his legs swell like balloons. Then they told him to ‘try harder.’
Meanwhile, the same people who cut these drugs are flying private to Dubai for their ‘wellness retreats.’
And yeah, mail order? Sure, if you got a stable address and a mailbox that ain’t been robbed since 2018. Try getting insulin delivered when you’re homeless and your phone dies every 3 hours.
This ain’t healthcare. It’s a rigged game where the house always wins - and you’re the chump paying with your life.