Metformin is the most prescribed diabetes medication in the world - and for good reason. It’s cheap, effective, and has been used safely for over 60 years. But if you’ve ever started metformin, you’ve probably heard the same stories: "It’ll wreck your stomach," "It’ll steal your B12," "You can’t take it forever." These aren’t just rumors - they’re myths that stick because they sound plausible. The truth? Most of them are outdated, exaggerated, or completely misunderstood. Let’s cut through the noise and look at what actually happens when you take metformin long-term.
Myth: Metformin Always Causes Severe Stomach Issues
It’s true - when you first start metformin, your stomach might rebel. Diarrhea, nausea, bloating - up to 30% of people experience these in the first few weeks. But here’s what no one tells you: those symptoms don’t last.
A 15-year study called the Diabetes Prevention Program Outcomes Study (DPPOS) tracked thousands of people on metformin. At the start, GI side effects were twice as common in the metformin group compared to placebo. But by year five? The gap closed. By year ten? There was no difference. Your body adapts. Most people who stick with it for more than six months report zero ongoing issues.
Why do some people struggle more? It’s often about how they start. Taking a full 1000mg dose on day one is like jumping into a cold pool. The recommended approach - backed by the American Diabetes Association - is to begin with 500mg once a day with dinner. Increase by 500mg every week until you reach your target dose. This slow ramp-up cuts discontinuation rates by more than two-thirds.
And if you’re still struggling? Switch to extended-release (XR). XR metformin releases the drug slowly over 24 hours, so your gut isn’t hit with a sudden surge. One study showed switching from immediate-release to XR cut diarrhea by more than half - from 18% to just 8%. Real people on Reddit and Diabetes Daily forums say the same thing: "I was miserable on regular metformin. Switched to XR once a day at night. Zero problems after two weeks."
Myth: Metformin Is Unsafe for Long-Term Use
"I heard metformin can cause lactic acidosis - it’s deadly." That’s the scariest myth, and it’s the one that makes some doctors hesitate. But here’s the reality: lactic acidosis from metformin is rarer than being struck by lightning.
According to FDA data, the risk is between 3 and 10 cases per 100,000 patient-years. That’s less than 0.01%. And every single one of those cases happened in people with serious, pre-existing conditions - like advanced kidney disease (eGFR below 30), liver failure, or severe heart failure. If your kidneys are working normally, metformin doesn’t build up. It doesn’t poison you. It just does its job: lowering liver sugar production and helping your muscles use insulin better.
The DPPOS study followed people on metformin for up to 15 years. No increase in cancer, no rise in heart problems, no hidden organ damage. Hemoglobin levels dipped slightly in the first year - but stabilized after that. Weight? People lost 2-3% of their body weight and kept it off. That’s more than most other diabetes pills can claim - and way better than the weight gain you get from insulin or sulfonylureas.
Metformin isn’t just safe for long-term use - it’s one of the most studied drugs in medical history. The American College of Physicians, the ADA, and the EASD all agree: if you’re starting medication for type 2 diabetes, metformin is still the best first choice.
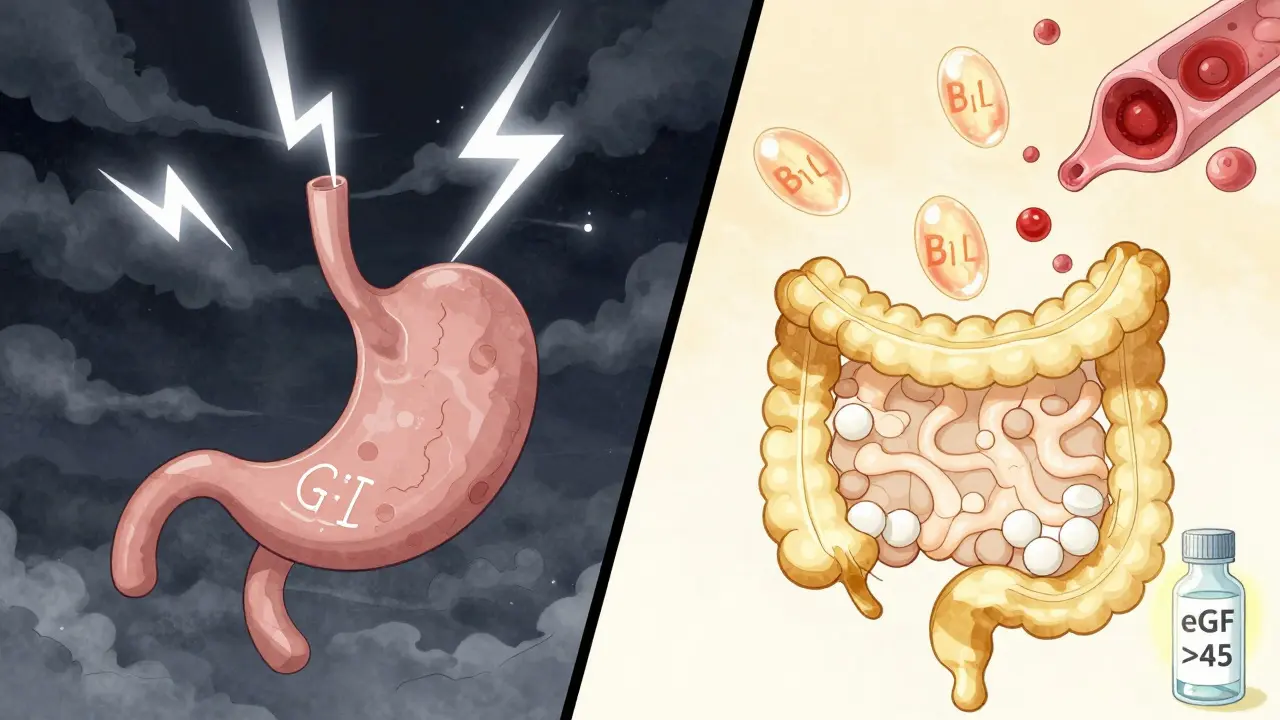
Myth: Metformin Doesn’t Affect Vitamin B12
This one’s sneaky. You won’t feel it. You won’t know it’s happening - until you start feeling tired, numb in your fingers, or having trouble thinking clearly. Metformin interferes with how your gut absorbs vitamin B12. The longer you take it, the bigger the drop.
A 2020 review of 17 studies found that after 4-12 years on metformin, people had, on average, 19% lower B12 levels than those not taking it. In some cases, levels dropped so low they caused true deficiency - affecting up to 30% of long-term users. That’s not rare. That’s expected.
Here’s the good news: it’s fixable. Unlike some side effects, B12 deficiency from metformin doesn’t mean you have to stop the drug. Just get your levels checked. The American Diabetes Association recommends testing every 2-3 years if you’ve been on metformin for more than four years - especially if you’re over 60, vegan, or have anemia or nerve pain (neuropathy).
If your levels are low, you don’t need fancy injections. High-dose oral B12 supplements (1000-2000 mcg daily) work just as well as shots for most people. A simple blood test, a $10 bottle of pills, and you’re back to normal. No need to panic. Just be aware.
Myth: Newer Diabetes Drugs Are Always Better Than Metformin
GLP-1 agonists like semaglutide (Wegovy, Ozempic) and SGLT2 inhibitors like empagliflozin (Jardiance) are getting all the attention. They help with weight loss. They protect your heart. They sound like magic bullets.
But here’s the catch: they cost 10-50 times more than metformin. A month of metformin? $4-$10. A month of Ozempic? $1000+ if you’re paying cash. And while those newer drugs have great benefits, they’re not necessarily better for everyone.
Metformin still wins on three things: cost, safety, and long-term data. No other diabetes pill has been studied for 15+ years in tens of thousands of people. No other pill has proven it can prevent diabetes in prediabetics. No other pill has been shown to lower death rates over decades.
That’s why, even in 2026, metformin is still the first-line drug for type 2 diabetes in 80% of U.S. clinics. Newer drugs are great additions - especially for people with heart disease or obesity - but they’re not replacements. Think of metformin as the foundation. The others are upgrades.

Myth: If You Can’t Tolerate Metformin, You Have No Options
Some people truly can’t take metformin - even with XR, even with slow titration. For them, the GI side effects are unbearable. But that doesn’t mean you’re stuck.
There are three smart alternatives:
- GLP-1 receptor agonists - like semaglutide or liraglutide. They’re injectable, but they help with weight, blood sugar, and heart health. Some people switch to these after failing metformin.
- SGLT2 inhibitors - like dapagliflozin or empagliflozin. Taken as pills, they help kidneys flush out sugar, lower blood pressure, and reduce heart failure risk.
- DPP-4 inhibitors - like sitagliptin. They’re weight-neutral and gentle on the stomach. Not as powerful as metformin, but very well tolerated.
The key? Don’t give up because one drug didn’t work. Work with your doctor. Try a different class. Your diabetes treatment isn’t a one-size-fits-all pill. It’s a toolkit.
What You Should Do Right Now
If you’re on metformin:
- If you’re still having stomach issues after 6 weeks, ask about switching to the extended-release version.
- If you’ve been on it for 4+ years, ask for a B12 blood test - even if you feel fine.
- If you’re worried about long-term safety, remember: your kidneys are the gatekeeper. Get your eGFR checked yearly. If it’s above 45, you’re fine.
- If you’re not on it yet but have prediabetes - ask if metformin is right for you. The DPP study showed it cuts diabetes risk by 31% over 10 years.
Metformin isn’t perfect. But it’s the most proven, most affordable, and most effective first step we have for type 2 diabetes. The myths around it are loud - but they’re not true. The facts? They’re solid.
Does metformin cause weight gain?
No. Unlike insulin or sulfonylureas, metformin is associated with modest weight loss - typically 2-3% of body weight over several years. It doesn’t make you hungry or store fat. In fact, it’s often chosen for people who need to lose weight.
Can I stop metformin if my blood sugar improves?
Maybe - but don’t stop without talking to your doctor. Some people with early type 2 diabetes can reduce or stop metformin after significant lifestyle changes - like losing weight or increasing activity. But stopping too soon can cause blood sugar to bounce back. Your doctor can help you decide if it’s safe to taper off.
Is metformin safe during pregnancy?
Metformin is often used during pregnancy for gestational diabetes or PCOS, especially when insulin isn’t preferred. Studies show it crosses the placenta but doesn’t increase birth defects. Many OB-GYNs consider it a safe option, though insulin remains the gold standard for tight blood sugar control in pregnancy.
Why do some people stop metformin after a few months?
Most stop because of temporary gastrointestinal side effects - nausea, diarrhea, bloating. These usually fade after 4-8 weeks. People who quit early often started too fast or didn’t switch to the extended-release version. Only about 4% of users discontinue due to side effects when dosed properly.
Does metformin damage the kidneys?
No. Metformin doesn’t harm healthy kidneys. In fact, it’s often used in people with early kidney disease (eGFR 30-45) under close monitoring. The risk comes from using it when kidneys are already severely damaged (eGFR below 30), where the drug can build up. That’s why doctors check kidney function yearly.


Comments
Lily Steele
I was on metformin for 5 years and never had a single stomach issue after switching to XR. Seriously, if you're struggling, just ask for it. It's a game changer.
Also got my B12 checked last year-was low as hell. Took 1000 mcg daily for a month and my energy came back. Simple fix.
Gaurav Meena
In India, metformin costs less than a cup of chai. People here call it 'diabetes ki dawai'-the diabetes medicine. And yeah, it works. No magic pills needed. Just science and patience. 🙏
Jodi Olson
The persistence of the lactic acidosis myth speaks to a deeper cultural anxiety about pharmaceuticals-our tendency to equate longevity of use with latent toxicity. Yet the data, robust and longitudinal, demonstrates a risk profile statistically indistinguishable from placebo in healthy populations. We must distinguish between pharmacokinetic concern and pharmacological fear.
Carolyn Whitehead
I started metformin last year and thought I was gonna die from the diarrhea. Switched to XR, took it at night, and now I barely remember I'm on it. B12 test? Yeah, I did that too. My doctor was like 'oh yeah, everyone should'. Easy peasy.
Amy Insalaco
The fact that you're still promoting metformin as first-line in 2026 is frankly archaic. The GLP-1 agonists have demonstrated not just glycemic control but cardiorenal protection, weight modulation, and even potential neuroprotective effects in preclinical models. Metformin is a 1950s-era molecule with a 1970s-era evidence base. We're optimizing for cost, not clinical superiority. It's not just outdated-it's a systemic failure of therapeutic innovation.
Katie and Nathan Milburn
Metformin has been used safely for over six decades. The clinical evidence is extensive, reproducible, and peer-reviewed across multiple continents. While newer agents offer adjunctive benefits, they do not invalidate the foundational role of metformin in metabolic management.
Beth Beltway
You say 'most people adapt' but what about the 20% who don't? You gloss over the fact that some of us have chronic diarrhea for years. And you act like B12 deficiency is just a 'check your levels' thing-like it's not causing permanent nerve damage if ignored. And you didn't mention the increased risk of gut dysbiosis. This is dangerously optimistic.
Marc Bains
I'm from Nigeria and we use metformin like it's aspirin. My cousin took it for 12 years, no problems. B12? We test it every year. Simple. Cheap. Works. Why make it complicated? The real issue is access-not the drug.
Melissa Cogswell
Just wanted to add: if you're on metformin and your eGFR drops below 45, don't panic. You don't have to stop it immediately. Many endocrinologists now use it down to eGFR 30 with close monitoring. Just talk to your doc. Don't self-discontinue.