Methadone QT Risk Calculator
This tool helps clinicians assess the risk of QT prolongation in patients taking methadone based on key factors including dose, medications, and clinical status.
Risk Assessment
When someone starts methadone for opioid use disorder or chronic pain, they’re not just taking a medication-they’re entering a complex web of biological interactions that can quietly turn life-threatening. The biggest hidden danger isn’t addiction or sedation. It’s what happens to their heart.
Why Methadone Is Different
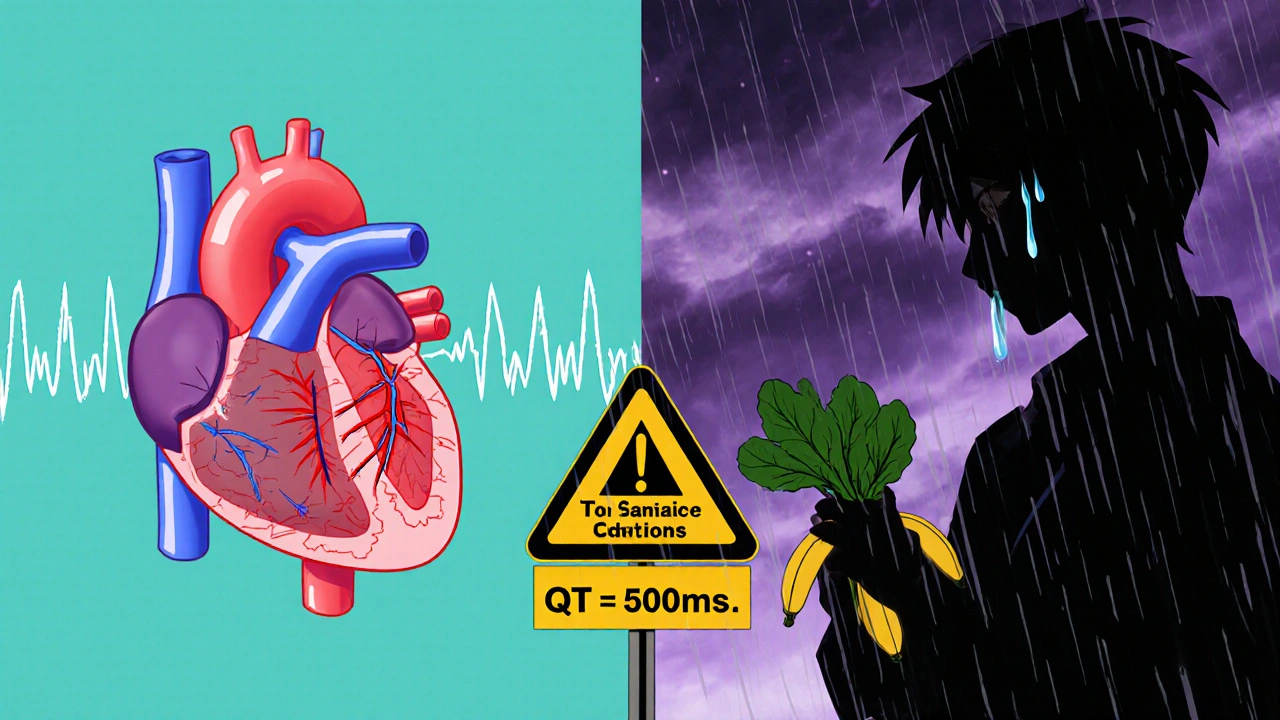
Methadone isn’t like other opioids. While drugs like oxycodone or buprenorphine mostly act on opioid receptors, methadone also blocks potassium channels in the heart-specifically the hERG channel. This slows down the heart’s electrical recovery phase, stretching out the QT interval on an ECG. A longer QT interval means the heart takes longer to reset between beats. That sounds harmless until it isn’t. When the interval gets too long, it can trigger a deadly rhythm called torsade de pointes, a type of ventricular tachycardia that can lead to sudden cardiac arrest.
The risk isn’t just theoretical. A 2007 study in JAMA Internal Medicine found that nearly 30% of patients on methadone had a QTc interval above 460 milliseconds-far beyond the safe limit. In that same group, over 16% had intervals over 500 ms, a level where the risk of sudden death jumps fourfold. What’s worse, this isn’t limited to high doses. Some patients on as little as 40 mg per day developed dangerous prolongation, especially if they had other risk factors.
The CYP Enzyme Trap
Methadone is broken down mostly by two liver enzymes: CYP3A4 and CYP2B6. If something blocks those enzymes, methadone builds up in the blood. That’s where the real danger kicks in. Many common medications are strong CYP3A4 inhibitors-and they’re often prescribed alongside methadone without anyone realizing the danger.
Fluoxetine (Prozac), clarithromycin (an antibiotic), fluconazole (a fungal treatment), and valproate (for seizures or mood) all interfere with methadone metabolism. When taken together, they can spike methadone serum levels by 30% to 50%. One patient on 80 mg of methadone might suddenly have levels equivalent to 120 mg. That’s not just a dose increase-it’s a cardiac time bomb.
Even worse, methadone itself can inhibit some of these same enzymes. That means the interaction isn’t always one-way. A patient taking fluconazole might not realize their methadone dose is now too high, and their doctor might not know to adjust it because the methadone level wasn’t checked.
Who’s at Highest Risk?
It’s not just about the dose. Risk comes from a perfect storm of factors:
- High methadone dose: Doses over 100 mg/day carry significantly higher risk, but dangerous QT prolongation has been seen at doses as low as 40 mg.
- CYP inhibitors: Fluoxetine, clarithromycin, fluconazole, ritonavir (in Paxlovid), and others.
- Low potassium: Hypokalemia directly worsens QT prolongation. Diuretics, vomiting, or poor nutrition can drop potassium levels.
- Heart disease: Previous heart attacks, heart failure, or congenital long QT syndrome.
- Female sex: Women naturally have longer QT intervals than men, making them more vulnerable.
- Liver problems: Reduced metabolism means methadone lingers longer.
A 2018 review of 32 cases of methadone-related torsade found that 57% of patients were taking at least one other QT-prolonging drug or CYP inhibitor. Nearly 40% had heart disease. One-third had low potassium. And yet, in nearly a third of cases, there was no clear link to methadone dose at all. That’s the problem-it’s unpredictable.

What Should Clinicians Do?
Guidelines have evolved. In 2023, the American Society of Addiction Medicine lowered the threshold for ECG monitoring from 100 mg/day to 50 mg/day. That’s because even lower doses can be dangerous when combined with other risk factors.
Here’s what works in practice:
- Baseline ECG before starting methadone. Measure QTc using the Bazett formula. Normal is ≤430 ms for men, ≤450 ms for women.
- Repeat ECG at stabilization. Usually after 2-4 weeks, or after any dose change.
- Check electrolytes. Especially potassium. Keep it above 4.0 mmol/L.
- Review all medications. Use a drug interaction checker. Avoid fluoxetine, clarithromycin, fluconazole, and ritonavir if possible. If you must use them, reduce methadone dose and monitor closely.
- Watch for symptoms. Dizziness, fainting, palpitations, or unexplained seizures could be early signs of torsade.
Some clinics now use electronic health record alerts that flag when a patient on methadone is prescribed a CYP3A4 inhibitor. That’s a game-changer. Without automation, these interactions slip through the cracks.
Buprenorphine vs. Methadone: The Cardiac Difference
Why is buprenorphine gaining ground? One major reason: it doesn’t prolong the QT interval. Studies show buprenorphine has minimal to no effect on cardiac repolarization, even at high doses. For patients with existing heart conditions, electrolyte imbalances, or those on multiple medications, buprenorphine is often the safer choice.
That doesn’t mean methadone should be abandoned. It’s more effective for some patients, especially those with high opioid tolerance. But the choice should be informed. If a patient has a history of arrhythmias, takes multiple medications, or has low potassium, switching to buprenorphine could prevent a cardiac event.
The Hidden Danger: New Drug Interactions
Most clinicians know about fluoxetine and clarithromycin. But what about Paxlovid? The antiviral combo of nirmatrelvir and ritonavir, used to treat COVID-19, contains ritonavir-a powerful CYP3A4 inhibitor. In 2022 and 2023, multiple case reports emerged of patients on methadone who developed severe QT prolongation after starting Paxlovid. One patient went from a normal QTc of 420 ms to 580 ms within three days. They needed emergency pacing.
Even over-the-counter drugs can be risky. Some antihistamines like diphenhydramine (Benadryl) and cimetidine (Tagamet) also prolong QT. Patients don’t always tell their doctors about these. That’s why a full medication review-prescription, OTC, supplements-is non-negotiable.
What Patients Need to Know
Patients on methadone should understand this: their heart is more sensitive than they think. They need to:
- Report any dizziness, fainting, or racing heartbeat immediately.
- Avoid starting new medications-including supplements-without checking with their provider.
- Know their baseline QTc and when their next ECG is due.
- Don’t skip potassium-rich foods (bananas, spinach, potatoes, beans).
- Understand that even after stopping a CYP inhibitor, methadone levels stay high for days due to its long half-life.
Many patients assume if they feel fine, they’re safe. But torsade can strike without warning. The goal isn’t to scare them-it’s to empower them with knowledge.
The Future: Personalized Risk Prediction
Researchers are now looking at genetics. Variants in the CYP2B6 gene affect how fast someone metabolizes methadone. Some people are slow metabolizers-meaning even standard doses can lead to buildup. A large NIDA-funded study (NCT04567812) is building a risk algorithm that combines genetics, age, sex, liver function, and medication list to predict who’s most at risk.
Soon, a patient’s genetic profile might tell their doctor whether they’re a high-risk candidate before methadone is even prescribed. Until then, caution is the only reliable tool.
Bottom Line
Methadone saves lives. But it can also end them-quietly, unpredictably, and often preventably. The biggest threat isn’t overdose. It’s the silent QT prolongation caused by drug interactions. Every patient on methadone needs an ECG before starting and again after stabilization. Every prescriber needs to check for CYP inhibitors. Every pharmacist needs to flag risky combinations. And every patient needs to know their heart is on the line.
There’s no magic bullet. But with careful monitoring, simple blood tests, and smart prescribing, the risk can be managed. The alternative? Another statistic in a CDC report. Another family losing someone to a death no one saw coming.
Can methadone cause sudden death even if the dose is low?
Yes. While higher doses increase risk, dangerous QT prolongation has been documented in patients on doses as low as 40 mg per day-especially when combined with CYP inhibitors like fluoxetine or fluconazole, low potassium, or heart disease. The interaction matters more than the dose alone.
What medications should be avoided with methadone?
Avoid CYP3A4 inhibitors like clarithromycin, fluconazole, ritonavir (in Paxlovid), and fluoxetine. Also avoid other QT-prolonging drugs such as certain antipsychotics (haloperidol, ziprasidone), antiarrhythmics (quinidine, sotalol), and some antibiotics (moxifloxacin). Always check drug interaction databases before adding any new medication.
How often should ECGs be done for someone on methadone?
A baseline ECG is required before starting methadone. A follow-up ECG should be done 2-4 weeks after starting or after any dose change. For patients on doses above 50 mg/day or with risk factors, ECGs should be repeated every 6-12 months. More frequent monitoring is needed if new medications are added or if potassium levels drop.
Is buprenorphine safer than methadone for the heart?
Yes. Unlike methadone, buprenorphine does not significantly prolong the QT interval, even at high doses. It’s often the preferred choice for patients with heart conditions, electrolyte imbalances, or those taking multiple medications that interact with CYP enzymes.
Can electrolyte imbalances make methadone more dangerous?
Absolutely. Low potassium (hypokalemia) and low magnesium directly worsen QT prolongation caused by methadone. Even mild imbalances can push a borderline QT interval into the danger zone. Regular blood tests for potassium and magnesium are essential for all patients on methadone, especially those on diuretics or with poor nutrition.


Comments
Zach Harrison
Man, I never realized how many everyday meds can mess with methadone. I had a buddy on it who got prescribed fluconazole for a yeast infection and ended up in the ER. No one told him it was dangerous. This post is a wake-up call.
Idolla Leboeuf
My cousin’s on methadone and she eats bananas like they’re candy now. She says her nurse told her potassium is her best friend. Smart move. Also ditched her Benadryl for sleep. No more sneaky OTC stuff.
M. Kyle Moseby
People need to stop being lazy. If you’re on methadone, get an ECG. That’s not optional. This isn’t a suggestion, it’s a lifesaver. Stop risking your heart because you’re too busy to schedule a doctor’s visit.
Elizabeth Nikole
They’re hiding this from us. I swear the system wants people to drop dead so they don’t have to pay for rehab. Paxlovid? They gave it to my uncle and he almost died. No warning. No nothing. This is murder by bureaucracy. 😡
Terri-Anne Whitehouse
Interesting that they cite the 2007 JAMA study but ignore the 2019 meta-analysis that found no significant increase in mortality below 120 mg/day when electrolytes are monitored. The fearmongering here is disproportionate to the actual data. Also, ‘QT prolongation’ isn’t a death sentence-it’s a biomarker. Context matters.
Halona Patrick Shaw
Bro. I was on 60mg for a year. No issues. Then my doc gave me clarithromycin for a sinus infection. Three days later I passed out in the shower. Turned out my QT was 520. I was lucky. I’m on buprenorphine now. No drama. No ECGs every other month. Just peace. Don’t let the system gamble with your heart.
Danny Pohflepp
Let’s be honest: this entire protocol is a controlled experiment. The FDA, pharmaceutical companies, and addiction clinics are all incentivized to keep patients on methadone because it’s profitable. The fact that buprenorphine is safer but less profitable? That’s not coincidence. That’s capitalism. They’re letting people die to maintain margins. And the ECGs? A performative gesture to avoid liability. Wake up.
Cole Brown
Hey, just wanted to say-this is super important info. If you’re on methadone, please, please, please talk to your pharmacist. They’re the ones who catch these interactions before your doctor even sees it. And don’t be shy about asking for a potassium test. It’s a simple blood draw. Worth every second. You’re worth it.