Blood Thinner & Pain Reliever Safety Checker
Check Your Medication Safety
This tool helps you understand if your blood thinner medication is safe to take with common pain relievers. Based on the latest medical research, it identifies dangerous combinations that increase bleeding risk.
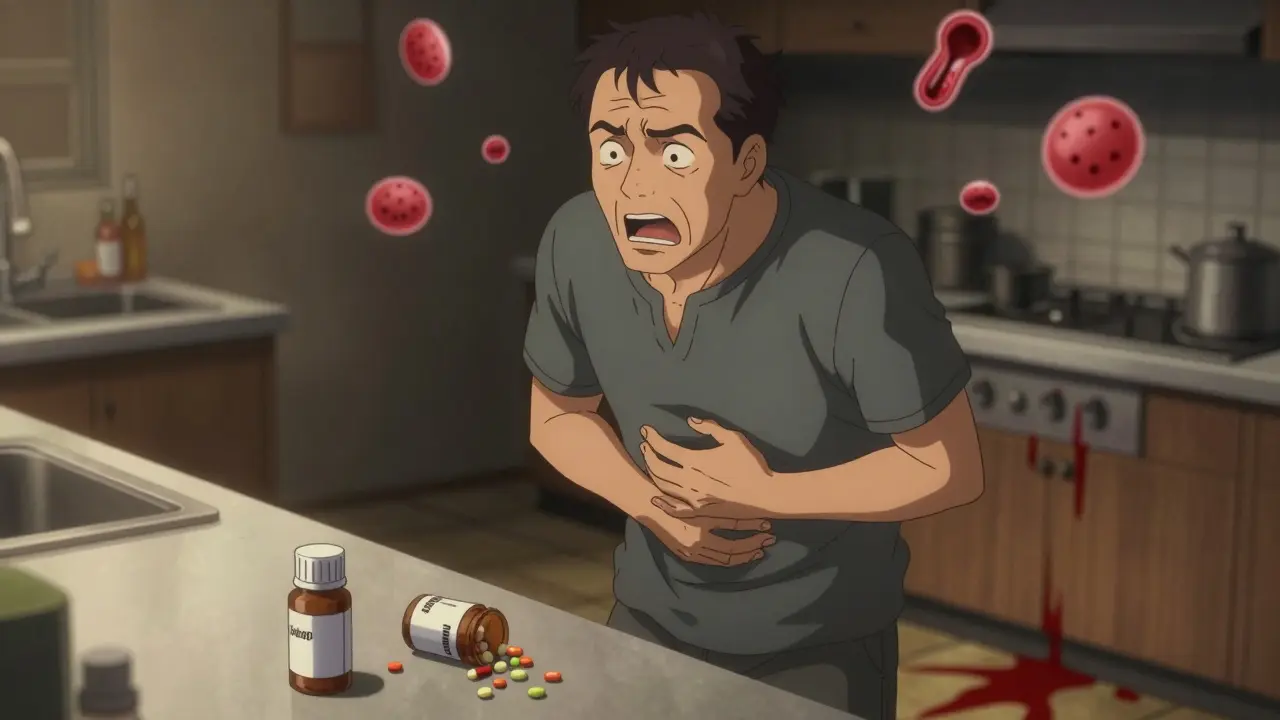
If you're taking a blood thinner like warfarin, apixaban, or rivaroxaban, and you reach for ibuprofen or naproxen to ease a headache, sore knee, or back pain, you're putting yourself at serious risk. This isn't a hypothetical warning-it's a well-documented, life-threatening interaction that sends tens of thousands of people to the emergency room every year. The combination of NSAIDs and blood thinners doesn't just add risks-it multiplies them.
Why This Combination Is So Dangerous
NSAIDs-like ibuprofen, naproxen, diclofenac, and even aspirin-work by blocking enzymes called COX-1 and COX-2. These enzymes help produce chemicals that cause inflammation and pain, but they also help platelets stick together to form clots. When you take an NSAID, your blood loses some of its ability to clot normally. At the same time, blood thinners like warfarin or DOACs (direct oral anticoagulants) slow down the actual clotting process by targeting proteins in your blood. When you put these two together, your body loses its ability to stop bleeding from even minor injuries.It's not just about cuts or bruises. The real danger lies in internal bleeding-especially in your stomach, brain, or intestines. A 2024 study from Denmark tracked over 120,000 people on blood thinners and found that those who took NSAIDs had more than double the risk of serious bleeding. Some NSAIDs were even worse: naproxen increased the risk by over four times, and diclofenac by more than three times.
Who’s Most at Risk?
This isn’t just a problem for older adults-it’s a crisis among them. About 12.1 million Americans over 65 take blood thinners, mostly for atrial fibrillation or deep vein clots. Many of them also have arthritis, back pain, or other chronic conditions that make NSAIDs seem like the obvious solution. But here’s the problem: nearly one in five of these patients take NSAIDs without telling their doctor. They grab a bottle from the cabinet, assume it’s safe because it’s over-the-counter, and don’t realize they’re playing Russian roulette with their internal organs.People with a history of ulcers, kidney disease, or high blood pressure are at even higher risk. The combination can also worsen anemia from slow, unnoticed bleeding. One study found that patients on both types of drugs were nearly three times more likely to develop anemia than those on blood thinners alone.
Not All Blood Thinners Are the Same
Some blood thinners are riskier than others when mixed with NSAIDs. Warfarin, the older drug, shows the strongest interaction. When taken with NSAIDs, it can cause your INR (a measure of how long your blood takes to clot) to spike by 0.8 to 1.2 points on average. That might sound small, but in clinical terms, it can push you from a safe range into dangerous territory where bleeding becomes likely.DOACs like apixaban, rivaroxaban, and dabigatran are generally safer than warfarin overall-but they’re still dangerous with NSAIDs. Studies show the bleeding risk with DOACs and NSAIDs is still 2 to 4 times higher than with DOACs alone. Even though DOACs don’t require regular blood tests like warfarin, that doesn’t mean they’re immune to this interaction. In fact, many patients assume DOACs are "safer," so they’re more likely to use NSAIDs without thinking twice.
What About Acetaminophen?
There’s one pain reliever that doesn’t mess with your blood’s clotting ability: acetaminophen (Tylenol). At standard doses-up to 4,000 mg per day-it’s the only over-the-counter option that won’t increase your bleeding risk. It doesn’t affect platelets or clotting factors. For people on blood thinners, it’s the go-to alternative.But it’s not perfect. Taking too much acetaminophen can damage your liver, especially if you drink alcohol or have existing liver problems. That’s why it’s not a one-size-fits-all solution. Still, for most people on blood thinners, it’s the safest bet for managing everyday pain.

The Hidden NSAIDs You Might Not Notice
Many people don’t realize they’re taking NSAIDs because they’re hiding in plain sight. Cold and flu medicines? Often contain ibuprofen or naproxen. Topical gels? Some have diclofenac. Even some menstrual pain relievers and migraine tablets are NSAIDs. One patient in a 2023 survey said she took a "cold medicine" for a stuffy nose and ended up in the ER with a stomach bleed. She didn’t even know the pill had ibuprofen in it.Dentists and physical therapists sometimes prescribe NSAIDs for post-procedure pain without checking if you’re on a blood thinner. That’s a major blind spot. In fact, 15% of FDA reports involving DOACs and bleeding events involved dental procedures where NSAIDs were given without proper screening.
What Should You Do Instead?
If you’re on a blood thinner and need pain relief, here’s what works:- Use acetaminophen as your first choice for headaches, muscle aches, or joint pain.
- Try non-medication options like heat packs, physical therapy, stretching, or massage. A 2023 Cleveland Clinic study found that 68% of patients on blood thinners were able to manage arthritis pain after four weeks of physical therapy-without any NSAIDs.
- If you absolutely must use an NSAID, talk to your doctor first. If approved, use the lowest dose possible (like 200 mg ibuprofen) for no more than three days, and always take it with a stomach-protecting drug like pantoprazole.
- Check every medicine label-even vitamins and supplements. Some herbal products like ginger, garlic, or ginkgo can also thin the blood.
Why Doctors Miss This
You’d think hospitals and clinics would flag this interaction automatically. But they don’t always. Only 38% of U.S. hospitals have electronic systems that block prescriptions for NSAIDs when a blood thinner is already on file. Most rely on doctors remembering to ask-and patients remembering to tell.Patients themselves often forget. One study found that only 29% of people could recall being warned about NSAIDs three months after their doctor’s visit. Another 47% didn’t even know the combination was dangerous, according to patient reviews on Drugs.com.
And then there’s the cost of ignoring this. In the U.S. alone, NSAID-blood thinner interactions cause 87,000 emergency room visits and 24,000 hospitalizations every year. The annual cost? Over $1.2 billion.

What’s Changing?
The tide is turning. The FDA is pushing for AI tools that automatically flag dangerous drug combinations before prescriptions are filled. Early tests show these tools catch 85% of risky pairings. The American Heart Association is expected to update its guidelines in early 2025, likely reinforcing the ban on NSAIDs for patients on long-term anticoagulants.Some hospitals are starting antithrombotic stewardship programs-dedicated teams that review all blood thinner prescriptions and flag risky interactions. In one 2024 study of 128 hospitals, these programs cut inappropriate NSAID use by 37%.
But until those systems are everywhere, the responsibility falls on you. If you’re on a blood thinner, assume every pain reliever is dangerous unless proven otherwise. Don’t trust the label. Don’t assume "over-the-counter" means "safe." And don’t wait for your doctor to ask-speak up.
Real Stories, Real Consequences
On Reddit’s r/Anticoagulants, 62% of over 1,400 respondents admitted to taking NSAIDs with their blood thinners. Over a third had experienced bleeding: nosebleeds, bruising, or worse. One man took ibuprofen after a tooth extraction while on apixaban. He bled for 14 hours straight and had to get a blood transfusion. Another woman took naproxen for her arthritis and ended up with a bleeding ulcer that required surgery.On the other side, patients who switched to acetaminophen and physical therapy reported better mobility, less pain, and no more hospital visits. One woman in Melbourne, who’s been on warfarin for atrial fibrillation, started seeing a physiotherapist twice a week. Within a month, she was walking without pain-and she hasn’t taken an NSAID in over two years.
Can I take ibuprofen with warfarin?
No. Taking ibuprofen with warfarin significantly increases your risk of dangerous bleeding, especially in the stomach and brain. Warfarin already makes your blood take longer to clot, and ibuprofen reduces your platelets' ability to form clots. Together, the risk multiplies. Even occasional use can lead to serious complications. Acetaminophen is the safer pain relief option.
Is naproxen safer than ibuprofen with blood thinners?
No. Naproxen is actually riskier than ibuprofen when combined with blood thinners. Studies show naproxen increases bleeding risk by over four times, while ibuprofen increases it by about 1.8 times. Both are dangerous. Neither should be used without explicit approval from your doctor-and even then, only for the shortest possible time.
What’s the safest painkiller if I’m on a blood thinner?
Acetaminophen (Tylenol) is the safest over-the-counter option. It doesn’t affect platelets or clotting factors like NSAIDs do. Stick to the recommended dose-no more than 4,000 mg per day-to avoid liver damage. For chronic pain, combine it with physical therapy, heat therapy, or other non-drug treatments.
Can I take NSAIDs occasionally if I’m on a DOAC like apixaban?
It’s not recommended. Even though DOACs like apixaban are safer than warfarin overall, combining them with NSAIDs still doubles or triples your bleeding risk. There’s no safe "occasional" use when the stakes are internal bleeding. If you must, talk to your doctor first. Use the lowest dose for no more than 2-3 days, and always take a stomach-protecting medication like pantoprazole.
How do I know if a medicine contains an NSAID?
Always read the "Active Ingredients" section on the label. Look for these names: ibuprofen, naproxen, diclofenac, ketoprofen, aspirin, celecoxib. They’re also in many cold, flu, and sinus medicines-sometimes listed as "pain reliever" or "anti-inflammatory." If you’re unsure, ask your pharmacist. Never assume a medicine is safe just because it’s sold over the counter.
What should I do if I accidentally took an NSAID while on a blood thinner?
If you took one dose and feel fine, monitor yourself closely for signs of bleeding: unusual bruising, dark or tarry stools, blood in urine, persistent nosebleeds, severe headaches, or dizziness. Call your doctor or go to the ER if any of these happen. Even if you feel okay, tell your doctor about the incident. They may want to check your blood clotting levels or adjust your medication.

Comments
Vikrant Sura
bro just take tylenol. why is this even a debate? the data’s right there. 87k er visits a year. that’s not a glitch, that’s a system failure.
Sai Keerthan Reddy Proddatoori
they say NSAIDs are dangerous but what about the big pharma lies? they push DOACs because they make more money. acetaminophen is old and cheap. they don’t want you to know.
Cara Hritz
i took ibuprofen for 3 weeks while on rivaroxaban and i’m fine?? maybe i’m just lucky? also i think the article overstates things. my dr never said anything.
Aliyu Sani
you know what’s wild? we treat pain like it’s a moral failing. like if you can’t endure it, you’re weak. but the body doesn’t care about stoicism-it just bleeds. NSAIDs aren’t villains, they’re bandaids on a ruptured artery. we need systems that don’t make patients guess if their headache is worth a stroke.
it’s not about fear. it’s about dignity. if you’re on a blood thinner, your pain deserves a safe solution-not a gamble.
and yet, we let pharmacists be the last line of defense? no wonder people end up in the ER. the system is designed to fail you before it even tries to help.
the real tragedy? the people who survive these interactions never talk about it. they just stop taking the meds. or worse-they stop trusting doctors entirely.
we need more than warnings. we need embedded checks. AI flags? good. but what about a mandatory 72-hour cooling-off period for NSAID scripts when anticoagulants are active? make it friction. make it intentional.
and for god’s sake, train dentists. how many people get a crown and walk out with a bottle of naproxen? that’s not care-that’s negligence dressed in scrubs.
acetaminophen isn’t perfect, but it’s the least terrible option. and if you’re still reaching for the blue bottle? you’re not reckless-you’re just uninformed. and that’s on us.
the fact that 47% of patients don’t even know this is dangerous? that’s not ignorance. that’s systemic abandonment.
we treat blood thinners like they’re just another pill. but they’re not. they’re a contract with your body. and NSAIDs? they’re the breach.
we need to stop treating this like a patient problem. it’s a healthcare design failure.
Jamison Kissh
the fact that we have to google whether a cold medicine contains ibuprofen is absurd. why isn’t there a universal color code? red for NSAIDs, green for safe? imagine if every OTC bottle had a little skull and crossbones if it interacts with anticoagulants.
we label everything else-allergens, caffeine, GMOs-but not this? this kills more people than most food recalls.
and why do we assume patients remember what their doctor said three months ago? memory is garbage. we need passive safeguards. like auto-blocks in pharmacy systems. if you’re on apixaban, you literally can’t check out with naproxen without a pharmacist override.
the 37% drop in NSAID use with stewardship programs? that’s proof we can fix this. we just need to stop treating it like an edge case.
Herman Rousseau
hey everyone-just wanna say this is one of the most important posts i’ve seen all year. 🙏
my dad was on warfarin for afib and took ibuprofen for his back. ended up with a GI bleed. spent 11 days in the hospital. he didn’t even know it was dangerous. now he only uses heat packs and Tylenol. he walks better than ever.
if you’re on a blood thinner and reading this? please, don’t wait for a scare. switch today. your future self will thank you. you’re not weak for needing relief-you’re smart for choosing safety.
Jeremy Hendriks
so let me get this straight-we’re telling people not to take a drug that works, because a different drug might kill them? what a brilliant paradox. if you can’t feel pain, you can’t feel alive. and if you feel alive, you might bleed out. beautiful. capitalism at its finest.
the real solution? stop prescribing blood thinners to old people. let nature take its course. less pills, less problems.
or better yet-just let the ER handle it. they’re already making bank off these interactions anyway.
Tarun Sharma
Thank you for this comprehensive overview. The data presented is compelling and aligns with clinical guidelines. Acetaminophen remains the recommended analgesic in this population. Further, non-pharmacological interventions should be prioritized as first-line options.
Kathryn Weymouth
the fact that 15% of DOAC-related bleeding events involve dental procedures is horrifying. dentists are supposed to be the first line of defense, not the last place you get poisoned. why aren’t they required to screen for anticoagulants before prescribing anything? it’s not rocket science.
i had a friend who got a tooth pulled and was handed ibuprofen. she didn’t say anything because she thought it was normal. she bled for two days. her dentist didn’t even ask if she was on blood thinners.
this isn’t just patient ignorance. it’s professional negligence.
Art Van Gelder
you ever notice how every time we fix one problem, another one pops up like a whack-a-mole? we got rid of warfarin’s constant blood tests, gave people DOACs, and now they think they’re invincible. "oh, it’s a new drug, so it’s fine!" no. it’s just a different kind of ticking bomb. and NSAIDs? they’re the match.
i live in the U.S., and honestly? we treat health like a buffet. take what you want, ignore the signs, hope for the best. but when you’re on a blood thinner, this ain’t a buffet. it’s a minefield.
and don’t get me started on the herbal "natural" stuff-ginger, garlic, ginkgo. people think because it’s from a plant, it’s safe. nah. nature doesn’t care if you’re on anticoagulants. it just wants you dead.
the woman in Melbourne who swapped naproxen for physio? that’s the future. that’s the win. not the ER. not the transfusion. not the ulcer surgery. the quiet, stubborn, daily choice to move your body instead of poisoning it.
we’ve forgotten that healing isn’t always a pill. sometimes it’s a stretch. sometimes it’s a massage. sometimes it’s just sitting still and listening to your body instead of drowning it in chemicals.
we need to stop treating pain like a problem to be erased. and start treating it like a signal to be understood.
Candy Cotton
As a former FDA compliance officer, I must emphasize that the data presented here is not only accurate-it is underreported. The 87,000 ER visits figure is conservative. Many cases are misclassified as "gastrointestinal hemorrhage" without noting the NSAID interaction. This is a public health crisis of systemic proportions. The current regulatory framework is woefully inadequate.
Sam Black
the quietest revolution in pain management isn’t a new drug-it’s the return to movement. when i started seeing a physiotherapist for my lower back, i didn’t just stop needing ibuprofen… i stopped hating my body. it’s not magic. it’s just… human. we were made to move, not medicate.
and yeah, Tylenol’s the safest bet-but don’t treat it like a crutch. pair it with heat, with breath, with time. your body’s smarter than your pharmacy shelf.
Jim Brown
There exists, in the architecture of modern pharmacology, a profound dissonance: we have engineered molecules of exquisite precision to prevent clotting, yet we continue to permit the casual, unregulated ingestion of agents that undermine their function with the casualness of a child reaching for candy. The NSAID-blood thinner interaction is not a pharmacological curiosity-it is a metaphysical indictment of our collective disregard for the sanctity of physiological boundaries. We have outsourced vigilance to algorithms, to pharmacists, to labels-but the body does not recognize bureaucracy. It bleeds. It remembers. And it does not forgive negligence disguised as convenience.