Beta-Blocker Risk Checker for Psoriasis
Most prescribed beta-blocker in the US
Linked to new-onset psoriasis
Linked to pustular psoriasis
Rarely prescribed, but high risk
Even topical use can trigger flares
If you have psoriasis and are taking a beta-blocker for high blood pressure or heart issues, your skin flare might not be random. It could be your medication.
What’s Really Going On Between Your Skin and Your Heart Med?
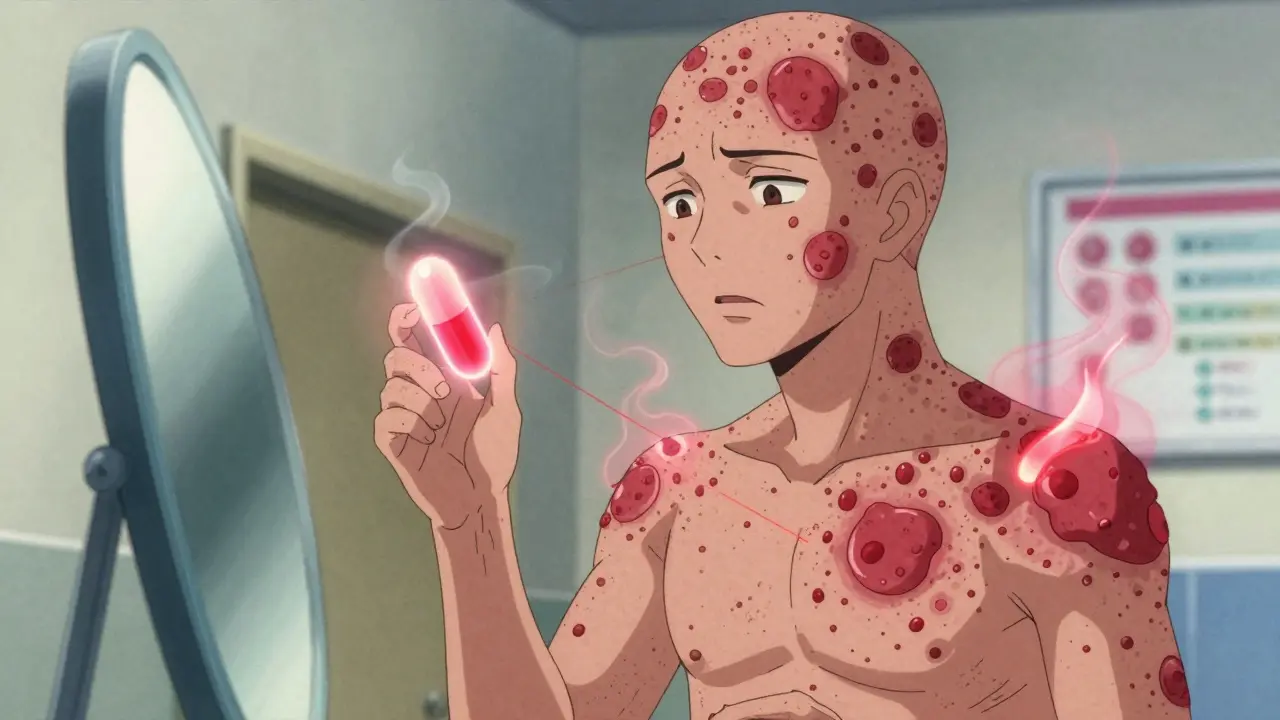
Psoriasis isn’t just a rash. It’s an autoimmune condition where your immune system attacks healthy skin cells, causing thick, scaly patches that itch, burn, or crack. About 8.1 million Americans live with it, and for many, triggers are unpredictable - stress, infections, weather changes. But one trigger that’s often missed? Beta-blockers. These drugs - like metoprolol, propranolol, and atenolol - are among the most common heart medications in the U.S., with over 63 million prescriptions filled last year alone. They work by slowing your heart rate and lowering blood pressure by blocking adrenaline. Simple, effective, life-saving for many. But for about 1 in 5 people with existing psoriasis, they also make skin symptoms worse. The connection isn’t new. Doctors have seen it since the 1970s, when a beta-blocker called practolol was pulled off the market because so many patients developed severe skin reactions. Today, even the newer versions - the ones still widely prescribed - carry the same risk.Which Beta-Blockers Are Most Likely to Trigger Flares?
Not all beta-blockers are created equal when it comes to skin effects. Some are far more likely to cause trouble:- Metoprolol (Lopressor, Toprol-XL) - the most prescribed beta-blocker in the U.S., and one of the top offenders for psoriasis flares.
- Propranolol (Inderal) - known to trigger both new-onset psoriasis and make existing cases much worse.
- Atenolol (Tenormin) - linked to pustular psoriasis, a more severe form with pus-filled bumps.
- Pindolol (Visken) - rare now, but has been tied to pustular psoriasis in case reports.
- Timolol (eye drops for glaucoma) - yes, even eye drops. The medication can be absorbed through the eye and trigger full-body psoriasis flare-ups.
How Do Beta-Blockers Even Affect Your Skin?
It’s not just coincidence. The science points to real biological changes. Beta-blockers reduce levels of a signaling molecule called cAMP inside skin cells. Lower cAMP means keratinocytes - the cells that make up your skin’s outer layer - start multiplying too fast. At the same time, immune cells in the skin get more active and inflamed. It’s like flipping two switches at once: one that speeds up skin cell production, and another that turns up the immune system’s heat. In people with psoriasis, this pushes an already overactive system into overdrive. Even worse, some beta-blockers may cause receptors in the skin to become less responsive over time, leading to a rebound effect that worsens inflammation. Studies show that patients who develop psoriasis after starting beta-blockers often see improvement - sometimes dramatic - after stopping the drug. That’s a key clue: if your skin gets better when you stop the medication, it’s likely the culprit.
Is It Causing Psoriasis - Or Just Making It Worse?
There’s debate here. Some studies say beta-blockers mainly worsen existing psoriasis. Others report cases where someone had no skin issues before - then started metoprolol for high blood pressure, and six months later, got full-blown plaque psoriasis. The American Academy of Dermatology says both can happen. But the stronger evidence points to worsening rather than causing outright. Still, if you’re genetically predisposed to psoriasis - say, you have a family history or carry the HLA-C*06:02 gene - your skin may be more vulnerable. A 2024 study at Johns Hopkins and Mayo Clinic is now looking at whether this gene can predict who’s at highest risk. Early results suggest carriers are far more likely to have a flare after starting a beta-blocker. That could one day mean genetic testing before prescribing.What Should You Do If You Suspect Your Med Is the Problem?
Don’t stop your beta-blocker on your own. These drugs are critical for heart health. Stopping suddenly can cause dangerous spikes in blood pressure or even heart attacks. Instead, do this:- Track your symptoms. When did the flare start? Did it get worse after starting the med? Did it improve after a dose change?
- Talk to both your dermatologist and cardiologist. They need to work together. Your skin doctor should ask, “Are you on any beta-blockers?” - and your heart doctor should know your psoriasis history.
- Consider alternatives. Calcium channel blockers like amlodipine or ARBs like losartan are often safer for psoriasis patients. ACE inhibitors (like lisinopril) can also trigger flares, so they’re not always a better choice.
- Try switching beta-blockers. If one triggers a flare, chances are others will too. Most doctors won’t recommend trying a different one.
What Happens If You Stop the Beta-Blocker?
Many patients see improvement within weeks to months after stopping the drug. One patient on Reddit reported his psoriasis went from covering 30% of his body to nearly gone after switching from metoprolol to a calcium channel blocker. Another said his flares cleared up after switching from propranolol to valsartan. But again - don’t quit cold turkey. Work with your doctors. They may slowly taper you off while introducing a new medication.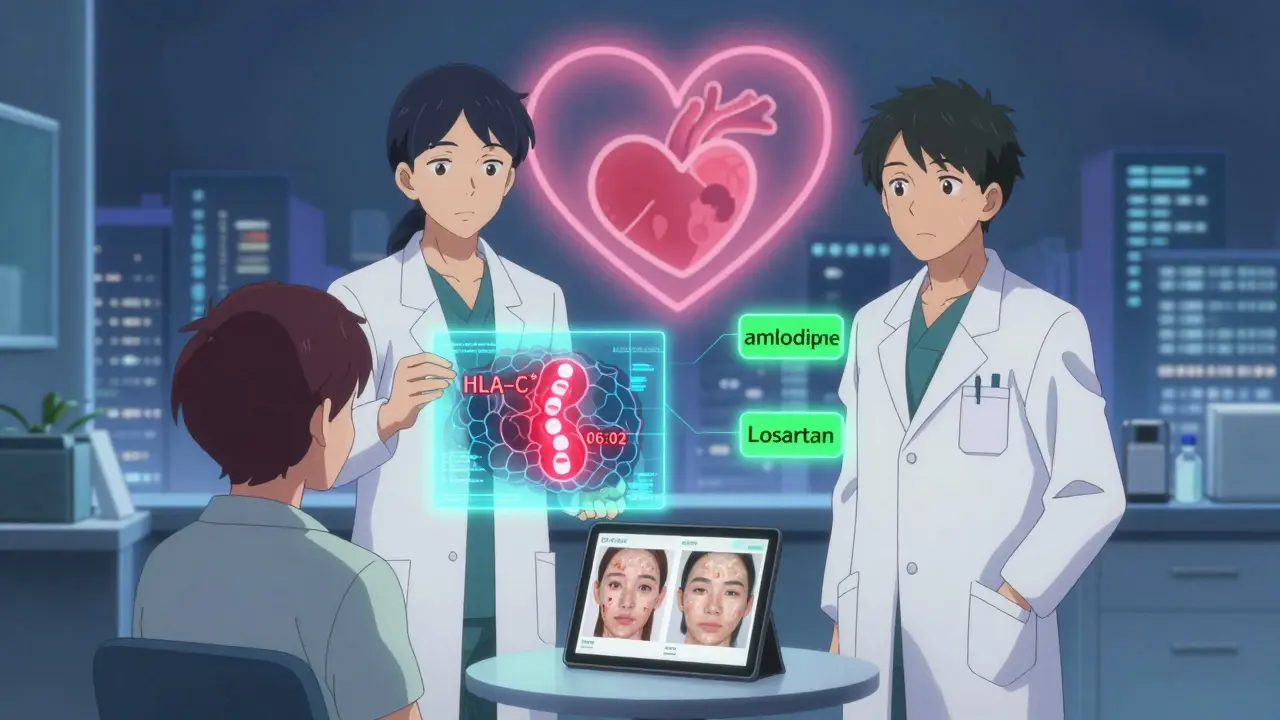
How Do You Manage the Flare in the Meantime?
While you’re adjusting meds, your dermatologist may recommend:- Topical corticosteroids to calm inflammation
- Vitamin D analogs like calcipotriene to slow skin cell growth
- Phototherapy (UV light treatment) for moderate to severe cases
- Systemic drugs like methotrexate or biologics if the flare is severe
Why This Matters More Than You Think
With 150 million beta-blocker prescriptions filled in the U.S. every year - and over 8 million people living with psoriasis - the overlap is huge. That means tens of thousands of people are likely being treated with heart meds that are making their skin condition worse. Most patients never connect the two. They see their dermatologist for the rash, their cardiologist for their blood pressure - and no one asks the right question: “Are you on any beta-blockers?” The European Academy of Dermatology now recommends that dermatologists ask this question during every new psoriasis evaluation. It’s a simple step - but it could prevent years of unnecessary suffering.Bottom Line: It’s Not All in Your Head - It’s in Your Meds
If you have psoriasis and are on a beta-blocker, your flare isn’t just bad luck. It’s a known, documented reaction. And while not everyone will be affected, the risk is real - especially if you’re on metoprolol, propranolol, or atenolol. The good news? You don’t have to choose between heart health and skin health. With the right team and the right alternatives, you can manage both. Talk to your doctors. Track your symptoms. Ask the question. Your skin might thank you.Can beta-blockers cause psoriasis for the first time?
Yes, in some cases. While beta-blockers are more commonly linked to worsening existing psoriasis, there are documented cases where people with no prior skin issues developed psoriasis after starting these medications - especially metoprolol and propranolol. The risk is lower than for flare-ups in existing patients, but it’s real.
How long after starting a beta-blocker does psoriasis usually flare up?
There’s no set timeline. Some people notice changes within weeks. Others don’t see a flare until 6, 12, or even 18 months after starting the medication. This delay makes it hard to connect the dots without a doctor’s guidance.
Is it safe to switch from one beta-blocker to another if one causes a flare?
Generally, no. If one beta-blocker triggers a psoriasis flare, others in the same class are likely to do the same. Most dermatologists and cardiologists recommend avoiding all beta-blockers in patients who’ve had a reaction, and switching to a different class of blood pressure medication instead.
Can eye drops with beta-blockers cause psoriasis?
Yes. Timolol eye drops, used for glaucoma, can be absorbed through the eye and enter the bloodstream. There are documented cases where these drops triggered full-body psoriasis or turned mild plaque psoriasis into severe erythroderma. If you have psoriasis and use eye drops, tell your dermatologist.
What are the safest blood pressure meds for people with psoriasis?
Calcium channel blockers like amlodipine and ARBs like losartan are generally considered safer for psoriasis patients. ACE inhibitors can also trigger flares, so they’re not always a better option. Your doctor will pick the best alternative based on your heart health, kidney function, and other conditions.
Do all psoriasis patients react to beta-blockers?
No. About 20% of people with psoriasis report worsening symptoms on beta-blockers. The rest may take them without any skin issues. Genetics, the specific drug, dosage, and overall immune health all play a role. If you’ve been on a beta-blocker for years with no flare, you’re likely in the majority who tolerate it fine.

Comments
Nancy Kou
This is one of those posts that should be mandatory reading for every dermatologist and cardiologist. I’ve been on metoprolol for five years and didn’t realize my flares were tied to it until I read this. Switched to amlodipine last month-my skin hasn’t looked this calm in years. No more midnight scratching, no more embarrassment at the pool. Doctors need to ask this question before writing prescriptions, not after you’re covered in scales.
Thank you for putting this out there.
Dev Sawner
It is imperative to note that the correlation between beta-blockers and psoriatic exacerbation has been empirically observed since the 1970s, and yet, clinical guidelines remain woefully inconsistent across jurisdictions. The pharmacokinetic mechanism involving cAMP suppression in keratinocytes is well-documented in peer-reviewed literature, yet primary care physicians continue to prescribe metoprolol as a first-line agent without screening for autoimmune predisposition. This is not merely negligence-it is systemic medical inertia.
Furthermore, the assertion that genetic markers like HLA-C*06:02 may predict susceptibility is not speculative; it is supported by GWAS data from the UK Biobank cohort. Until mandatory genetic screening is implemented for all patients prescribed beta-blockers, we are engaging in dangerous trial-and-error medicine.
Andrew Kelly
Let’s be real-this isn’t about beta-blockers. It’s about Big Pharma pushing drugs that make people sick so they can sell more creams and biologics. You think they care if your skin flares? They make billions off the side effects. The real culprit? The FDA letting these drugs stay on the market for decades while they quietly bury the data.
And don’t get me started on ‘alternatives’ like amlodipine-those cause ankle swelling and gout. You’re just trading one problem for another. The system is rigged. Your doctor doesn’t know what’s going on. Neither do you. You’re just a walking profit margin.
Connie Zehner
OMG I’m crying. 😭 I’ve had psoriasis since I was 12 and was on propranolol for anxiety for 3 years. My whole back turned into a red, scaly mess. I thought I was just stressed. Turns out it was the meds. I switched to sertraline and my skin cleared up in 6 weeks. I wish I’d known this sooner. Why doesn’t anyone tell you this stuff before you start the pills?
Also-my mom has glaucoma and uses timolol drops. I just screamed at her to stop. She’s not listening. I’m so scared for her. 😭
Hussien SLeiman
Of course the medical establishment ignores this. They don’t want to admit that their golden child drugs-beta-blockers-are causing chronic disease in millions. It’s not just psoriasis either. I’ve seen the same pattern with lupus, rheumatoid arthritis, even alopecia areata. The moment someone starts a beta-blocker, their immune system goes rogue.
And let’s not pretend that switching to a calcium channel blocker is some magical fix. Those cause dizziness, edema, constipation, and sometimes arrhythmias. You’re just swapping one set of side effects for another. The real solution? Lifestyle. Diet. Stress reduction. Get off the pills entirely. The body doesn’t need synthetic adrenaline blockers to survive. It needs rest, clean food, and sunlight. But no, we’d rather pop a pill and call it a day.
And don’t get me started on biologics. $10,000 a month to suppress your immune system while the root cause-your meds-remains untouched. This isn’t medicine. It’s a business model built on perpetual suffering.
Meenakshi Jaiswal
Hi everyone-I’m a dermatology nurse with 12 years of experience. I’ve seen this exact pattern over and over: patient comes in with worsening plaques, we dig into meds, and it’s always metoprolol or propranolol. I’ve had patients go from 40% body surface area involvement to under 5% after switching meds.
Here’s what I tell everyone: Track your flares. Write down when you started the med, when the itching started, when the scaling spread. Bring it to both your derm and your cardiologist. They’re not talking to each other-so you have to be the bridge.
And yes, amlodipine and losartan are safer. But if you have heart failure or post-MI, sometimes you need a beta-blocker. In those cases, carvedilol might be a better option-it has less skin impact. Always ask for alternatives. You’re not being difficult. You’re being smart.
Mahammad Muradov
It is a well-established fact that beta-blockers induce psoriasiform eruptions via downregulation of cyclic adenosine monophosphate in epidermal keratinocytes, thereby accelerating cellular turnover and amplifying Th17-mediated inflammation. The clinical relevance of this phenomenon is statistically significant in meta-analyses with p-values < 0.001.
However, the notion that switching to ARBs constitutes a therapeutic solution is empirically unsound. Losartan has been associated with angioedema in patients with C1 esterase inhibitor deficiency, a comorbidity not uncommon in psoriatic populations. Furthermore, calcium channel blockers may exacerbate peripheral vascular disease, which is frequently comorbid with metabolic syndrome in this cohort.
Therefore, the optimal management strategy requires individualized risk stratification based on cardiovascular risk profile, HLA typing, and renal function-not arbitrary drug substitution. To suggest otherwise is to engage in clinical oversimplification.
Moses Odumbe
Bro. I was on metoprolol for 2 years. My scalp was flaking like a snow globe. I thought I had dandruff. Then I switched to lisinopril. Still broke out. Then I switched to verapamil. Skin cleared up in 3 weeks. No joke. My dermatologist didn’t even know this was a thing. I had to Google it myself.
PSA: If you’re on ANY beta-blocker and your skin sucks-ask your doc about switching. Don’t wait. It’s not ‘just stress.’ It’s the pill.
Also-emoji for truth: 🚨💊➡️🧂
holly Sinclair
What does it mean when medicine treats symptoms as isolated events rather than manifestations of systemic imbalance? We’ve turned the body into a machine with interchangeable parts-pop a pill for blood pressure, another for skin, another for sleep-and never ask why the whole system is failing.
Beta-blockers suppress adrenaline, sure-but what if the body needed that adrenaline to regulate immune signaling? What if the real problem isn’t the drug, but the chronic stress, poor sleep, and inflammation that drove us to need the drug in the first place?
Maybe the skin flare isn’t a side effect. Maybe it’s a signal. A message from the body saying, ‘You’re not living in alignment.’ We treat the symptom, not the source. And we wonder why nothing ever really gets better.
Is it possible that the most effective treatment isn’t a different pill… but a different life?
Isabel Rábago
I don’t care what the studies say. If you’re taking beta-blockers and you have psoriasis, you’re just not trying hard enough to manage your stress. I’ve had psoriasis my whole life and I’ve never taken a beta-blocker. I eat clean, meditate, walk daily. My skin is fine. Stop blaming your meds. Take responsibility.
Also, your doctor isn’t lying to you. You’re just looking for an excuse.