Switching from a brand-name drug to a generic version seems like a simple cost-saving move. But for some people, that switch triggers headaches, anxiety, seizures, or worse. And it’s not just in their head. There’s real, documented evidence that for certain medications, changing the manufacturer-even when it’s labeled "therapeutically equivalent"-can cause serious problems.
Why switching generics isn’t always harmless
The FDA says generics are just as safe and effective as brand-name drugs. And for most people, that’s true. But the agency allows up to a 20% difference in how quickly the body absorbs the active ingredient between a brand-name drug and its generic version. That’s not a typo. It means two different generics of the same drug could be up to 45% apart in absorption rates. For drugs like statins or antibiotics, that’s usually fine. But for others, even a small change can be dangerous. The real risk comes with drugs that have a narrow therapeutic index (NTI). These are medications where the difference between a helpful dose and a toxic one is tiny. A little too much, and you get side effects. A little too little, and the drug doesn’t work. That’s why switching generics for these drugs can feel like playing Russian roulette with your health.Which drugs are most risky to switch?
Not all generics are created equal. Some drug classes have a long history of problems when switched. Here are the top five:- Antiepileptics - Drugs like phenytoin, lamotrigine, and extended-release divalproex sodium. A 2021 survey of 147 neurologists found that 68.7% believed switching generics increased seizure risk. One patient reported having breakthrough seizures within days of switching from one generic to another.
- Thyroid medication - Levothyroxine. Even tiny changes in absorption can throw your metabolism out of balance. Symptoms? Fatigue, weight gain, heart palpitations, or anxiety. The FDA itself acknowledges that levothyroxine is a special case, and many doctors now write "dispense as written" on prescriptions to prevent automatic substitution.
- Anticoagulants - Warfarin. A 2019 study in BMJ Open showed a 12.3% higher risk of hospitalization within 30 days of switching between generic warfarin products. INR levels can swing dangerously, leading to clots or bleeding.
- Immunosuppressants - Tacrolimus and cyclosporine. For transplant patients, a drop in drug levels can trigger organ rejection. A single switch has been linked to graft failure in multiple case reports.
- Psychiatric medications - Especially extended-release ADHD drugs like Adderall XR and antidepressants like bupropion XL. Patients report sudden return of symptoms, new anxiety, insomnia, or mood swings within 24-72 hours of switching. A 2023 Reddit thread with over 800 comments from ADHD patients described the same pattern: "My focus vanished. My anxiety spiked. I felt like I was back in high school again."
What’s really changing between generics?
You might think all generics are the same because they contain the same active ingredient. But what’s inside the pill matters more than you’d expect. The inactive ingredients-fillers, binders, coatings, and time-release beads-can vary wildly between manufacturers. These don’t treat your condition, but they control how and when the active drug is released. For example, Adderall XR uses tiny beads that release medication at different times. One generic version might use a different coating that dissolves faster, causing a spike in blood levels. Another might release too slowly, leaving you without symptom control by midday. Both meet FDA bioequivalence standards. But your brain doesn’t care about the standards-it only cares about how you feel. A 2023 hospital study found that 67% of patients identified their meds by color and shape. When those changed, many didn’t realize they’d been switched. Some even took both versions, thinking they were different pills, leading to accidental overdose. One case ended in serotonin syndrome-requiring emergency hospitalization.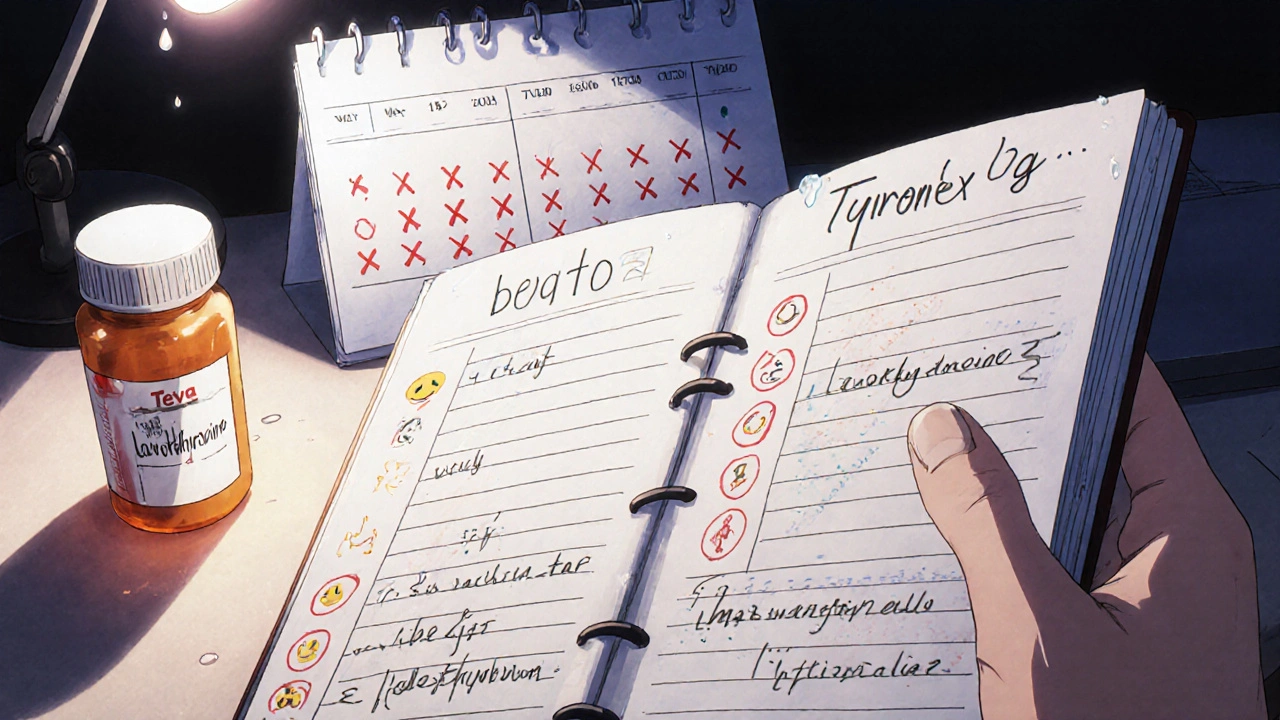
Why do switches happen so often?
It’s not about your health. It’s about money. Pharmacy benefit managers (PBMs)-companies like CVS Caremark and Express Scripts-control which generics pharmacies stock. They make deals with manufacturers: the one offering the biggest rebate gets placed on the preferred list. That list changes every few months. So your prescription might come from one generic maker this month, another next month, and a third the month after. According to a 2022 Senate investigation, PBMs switch preferred generic manufacturers an average of 4.7 times per year per drug. For psychiatric meds, that’s 76.4% of patients getting switched at least once a year. The FDA’s Orange Book lists 12 different generic versions of levothyroxine alone. No wonder patients are confused-and sometimes harmed.When should you worry?
You should pay attention if you notice any of these after a switch:- New or worsening side effects (headaches, dizziness, nausea, anxiety, insomnia)
- Return of symptoms you had under control (seizures, panic attacks, fatigue, brain fog)
- Unexplained changes in lab results (INR for warfarin, TSH for thyroid meds)
- Feeling "off" without a clear reason

What you can do to protect yourself
You don’t have to accept random switches as normal. Here’s how to take control:- Ask for the manufacturer name when you pick up your prescription. Pharmacists can often fill your script with the same brand if you ask. Write down the name (e.g., "Mylan" or "Teva") so you recognize it next time.
- Keep a medication log - Note the drug name, dose, manufacturer, and any side effects or changes in how you feel. Do this for 72 hours after every refill. This helps you spot patterns.
- Ask your doctor to write "DAW 1" on your prescription. That means "dispense as written"-no substitutions allowed. This is especially important for NTI drugs.
- Talk to your pharmacist - Ask if the generic you’re getting is the same as last time. If it’s not, ask why and whether you can stick with the one that works.
- Report side effects - If you notice a problem after a switch, tell your doctor and file a report with the FDA’s MedWatch program. Your report helps others.
What’s changing in the system?
There’s growing recognition that this isn’t just a minor annoyance-it’s a patient safety issue. In 2023, Medicare Part D rules changed to limit generic switches to no more than twice a year. That’s a start. The FDA launched a $15.7 million initiative to improve testing for complex generics like inhalers and extended-release pills. In January 2024, the American Society of Health-System Pharmacists published a list of 17 drugs where automatic substitution should be avoided, including bupropion XL and tacrolimus. But the biggest change? More doctors and patients are speaking up. A 2024 study found that CYP2D6 poor metabolizers-people whose bodies process certain drugs slowly-are 4.2 times more likely to have treatment failure after a generic switch. That’s not random. It’s genetic. And it’s being ignored.The bottom line
Generics save billions. That’s good. But not at the cost of your health. If you’re on a high-risk medication and you feel different after a refill, it’s not in your head. It’s the pill. You don’t need to fight the system alone. You just need to be informed, speak up, and track your symptoms. Your body knows when something’s wrong. Listen to it.Are generic drugs always safe to switch to?
For most people and most medications, yes. But for drugs with a narrow therapeutic index-like thyroid meds, seizure drugs, blood thinners, and some psychiatric medications-even small changes in formulation can cause serious side effects or loss of effectiveness. Switching isn’t always harmless.
Why do I feel worse after switching to a generic?
The active ingredient is the same, but the inactive ingredients-fillers, coatings, and time-release beads-can differ between manufacturers. These affect how fast the drug enters your bloodstream. For sensitive individuals, even a 10-20% difference in absorption can trigger symptoms like anxiety, headaches, fatigue, or return of original conditions like seizures or depression.
Can my pharmacist tell me which generic manufacturer I’m getting?
Yes. The manufacturer name is printed on the bottle or packaging. You can ask your pharmacist to tell you which company made your pills-and request the same one next time. Many pharmacies can accommodate this if you ask.
What does "DAW 1" mean on a prescription?
"DAW 1" stands for "Dispense As Written." It means the doctor doesn’t want any substitutions-your prescription must be filled with the exact brand or generic they prescribed. This is especially important for high-risk drugs like levothyroxine or tacrolimus. Ask your doctor to include this code if you’ve had bad reactions to switches.
Should I avoid generics altogether?
No. Generics are safe and effective for most people and most medications. But if you’re on a drug with a narrow therapeutic index-or if you’ve had problems after a switch before-ask for consistency. Don’t let cost savings override your health. Work with your doctor and pharmacist to find a stable, safe option.
How common are side effects from switching generics?
For high-risk drugs, it’s more common than you think. A 2023 hospital study found 20% of patients on frequently switched medications experienced side effects from accidental duplication or formulation changes. In ADHD patients, 63% reported reduced effectiveness after a generic switch. These aren’t rare cases-they’re warning signs.
Can I switch back to my original generic?
Yes. If you notice side effects or reduced effectiveness after a switch, contact your pharmacist and doctor. They can often request the previous manufacturer’s version. Some pharmacies keep stock of multiple generics. Don’t wait until you’re in crisis-act as soon as you notice a change.


Comments
Paul Baker
bro i switched my levothyroxine last month and woke up feeling like a zombie 🥱💸 now i know why my weight went up 10lbs in 2 weeks
Jeremy S.
this is real. my cousin had seizures after a generic switch. don't ignore it.
Kristy Sanchez
oh so now the pharmaceutical industry is secretly running a human experiment on us? shocking. 🙄 btw i'm pretty sure your 'narrow therapeutic index' is just your body being weak. maybe try yoga?
Jeremy Mattocks
I’ve been a pharmacist for 22 years and let me tell you - this isn’t some conspiracy. The FDA’s 20% bioequivalence window is a legal loophole, not a safety standard. For drugs like warfarin or tacrolimus, that variance isn’t just theoretical - I’ve seen patients bleed out or reject transplants because their pill changed color. And no, the pharmacist doesn’t always tell you. The label says ‘generic’ and that’s it. You’re supposed to just trust it. Meanwhile, PBMs are juggling rebates like it’s a game of musical chairs, and you’re the one sitting on the wrong chair when the music stops. I’ve had patients come in with five different bottles of the same drug because they didn’t realize they’d been switched. One guy took both - thought they were different strengths. Ended up in the ER with serotonin syndrome. The inactive ingredients? They’re not inert. They’re the reason your extended-release pill doesn’t turn into a time bomb at 3 p.m. And yes, the color and shape matter. Your brain recognizes those cues. Change them, and your body panics. This isn’t about being paranoid. It’s about being informed. Ask for DAW 1. Write down the manufacturer. Track your symptoms. And if your doctor shrugs? Get a new one. Your life isn’t a cost-cutting spreadsheet.
Jill Ann Hays
The systemic failure of pharmaceutical regulation to account for inter-individual pharmacokinetic variability represents a profound ethical breach in public health policy. The FDA's bioequivalence thresholds were established during an era of simplistic pharmacological models and fail to accommodate the complex polygenic expression profiles observed in modern populations. Consequently, the current paradigm of generic substitution constitutes an epistemic injustice against patients who possess metabolic phenotypes incompatible with standardized release kinetics
Sarah McCabe
i had the same thing with my antidepressant 😔 switched generics and felt like i was drowning in slow motion. took me 3 weeks to figure out it was the pill. now i only take the blue ones. 🌊💙
King Splinter
so let me get this straight - you’re saying that a pill that’s chemically identical can make you feel different? wow. what a shocker. next you’ll tell me water can be wet. this whole thing is just people being dramatic because they don’t like change. also i take generic Adderall and i’m fine so your experience is invalid
Michael Friend
The data is cherry-picked. The BMJ study showed a 12.3% increase in hospitalizations - but correlation isn't causation. You're ignoring confounding variables: patient noncompliance, co-morbidities, concurrent medication changes, and the placebo/nocebo effect. The FDA's bioequivalence standards are among the most rigorously validated in the world. To suggest otherwise is to undermine public trust in evidence-based medicine and embolden anti-pharma sentiment without data.
Dominic Fuchs
you know what’s funny? the same people who scream about generic switches are the ones who’ll buy $800 insulin because they think brand name = better. it’s not about the pill. it’s about control. you want to believe your body is too special for mass-produced medicine. but here’s the truth - most people are fine. the rest? they’re just not getting the right dose. fix that, not the manufacturer
Asbury (Ash) Taylor
This is an incredibly important discussion. Thank you for bringing attention to the systemic issues in pharmacy benefit management. I’ve worked with transplant patients for over a decade, and the anxiety they experience when their tacrolimus changes is palpable. The FDA needs to establish tiered bioequivalence standards for NTI drugs - not a one-size-fits-all approach. Patient safety must override rebate structures. This isn’t anti-generic. It’s pro-patient.
Kenneth Lewis
i switched my bupropion and thought i was having a breakdown 😭 turned out my new generic had a different coating - took me 2 weeks to figure it out. now i take a pic of the pill every time. it’s dumb but it works
Zack Harmon
THIS IS A MASS MURDER SCHEME. THEY’RE KILLING US WITH CHEAP PILLS. MY FRIEND’S KID HAD A SEIZURE BECAUSE SOME CORPORATE BEAN COUNTER SAVED 3 CENTS. THIS ISN’T HEALTHCARE - IT’S A GAME OF CHICKEN WITH DEADLINES. THE FDA IS COMPlicit. THE PHARMACIES ARE IN ON IT. WE NEED A REVOLUTION. #GENERICMURDER
Jerrod Davis
The assertion that pharmaceutical substitution may result in clinically significant pharmacokinetic variation is not supported by the totality of peer-reviewed literature. The bioequivalence paradigm, as codified under 21 CFR 320.23, has demonstrated robust reproducibility across over 1,200 generic approvals. Anecdotal reports, while emotionally compelling, do not constitute evidence of systemic failure. To recommend DAW-1 as a standard practice is to promote therapeutic inertia and undermine cost-containment initiatives essential to sustainable healthcare delivery.
Jim Daly
i dont care what the fda says. if my pill looks different i dont take it. i dont trust these companies. they dont care about me. i’d rather pay 3x and know its the same one. its not about money its about peace of mind. also my cousin died from a generic switch. true story.