When a patient gets a prescription for a generic version of a high-cost specialty drug, many assume it’s just like picking up a generic pill at the corner pharmacy. But that’s not how it works. Even when the drug is no longer branded, the process stays locked inside the specialty pharmacy system - and providers play a critical role in making sure it gets done right.
Why Generic Specialty Drugs Still Need Specialty Pharmacies
You might think that if a drug becomes generic, it loses its complexity. Not true. Specialty drugs - whether brand or generic - are defined by how they’re used, not just what’s in the bottle. These are medications that need special handling: refrigeration, IV infusion, strict dosing schedules, or constant monitoring for side effects. Think drugs for rheumatoid arthritis, multiple sclerosis, cancer, or hepatitis C. Even when a generic version hits the market, the same rules apply. The FDA doesn’t approve true generic copies of biologic drugs like Humira or Enbrel. Instead, they approve biosimilars - highly similar versions that still require the same precision in storage, administration, and patient follow-up. And manufacturers don’t allow retail pharmacies to dispense them. Even if it’s a generic small-molecule specialty drug, like methotrexate for autoimmune conditions, if the manufacturer designates it for specialty distribution, only specialty pharmacies can fill it. It’s not about the cost - it’s about control.The Provider’s Role: More Than Just Filling Prescriptions
Providers - doctors, nurse practitioners, and pharmacists - are the backbone of this system. They don’t just write prescriptions. They make sure the right patient gets the right drug at the right time, with the right support. First, they verify the prescription. That means checking the diagnosis matches the drug’s FDA-approved use. Then they handle prior authorization. This isn’t a quick form. It’s a back-and-forth with insurers, often requiring lab results, treatment history, and proof that cheaper alternatives failed. For generic specialty drugs, insurers sometimes still require this step - even if the drug is cheaper - because they’re wary of therapeutic substitution. Next comes patient education. A provider or care coordinator explains how to inject the drug, what side effects to watch for, and when to call for help. They don’t just hand over a bottle. They schedule follow-up calls. They track lab results. They coordinate with nurses who visit patients at home. One patient on Reddit said, “My generic version of Xeljanz still comes with the same nurse who knows my whole history. That’s why I stay.” That relationship matters.How the System Works - Step by Step
The workflow for dispensing generic specialty drugs is the same as for branded ones:- Prescription intake - Received electronically or by fax, checked for accuracy and eligibility.
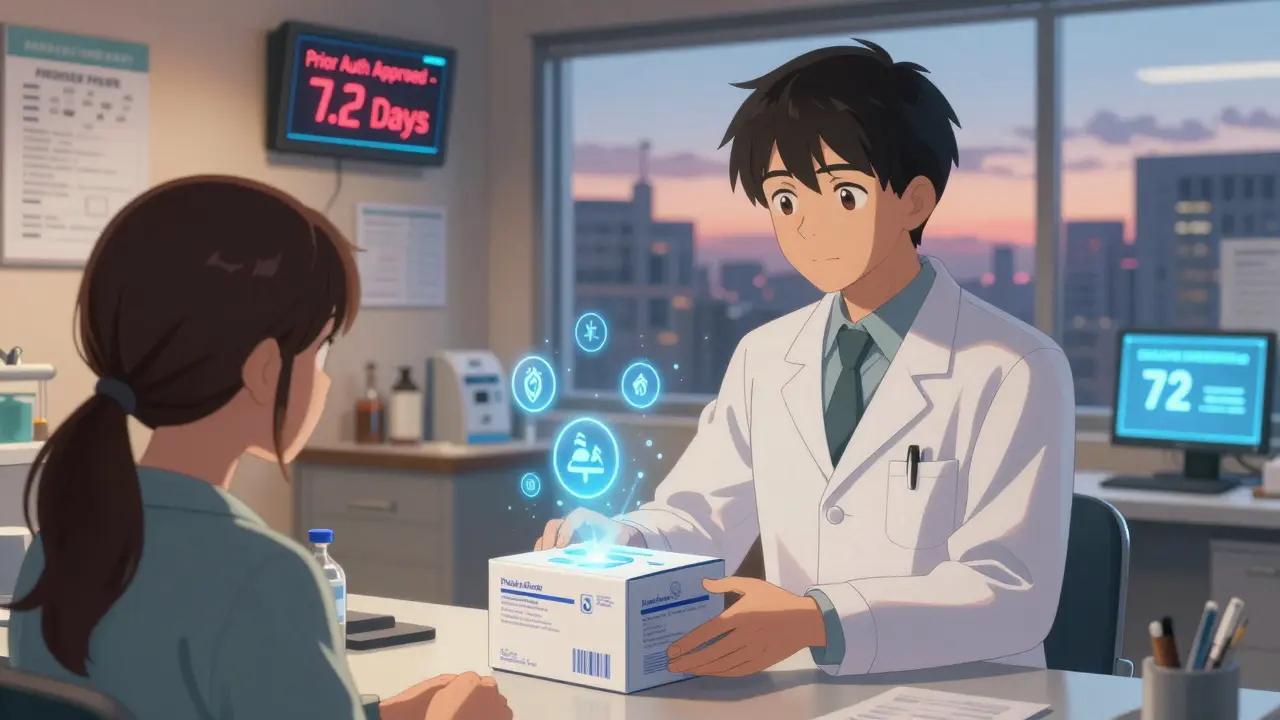
- Prior authorization - Submitted to insurer with clinical documentation. Takes 3-10 days on average.
- Financial assistance - Providers help patients apply for copay cards or manufacturer aid programs. Even generics can cost hundreds per month.
- Clinical review - Pharmacist checks for drug interactions, allergies, and dosing appropriateness.
- Dispensing - Packaged in temperature-controlled containers with detailed instructions.
- Delivery - Shipped via overnight courier with tracking and signature confirmation.
- Follow-up - Patient contacted within 48 hours to confirm receipt and answer questions.
Why Retail Pharmacies Can’t Handle These Drugs
You might wonder: why not just use Walgreens or CVS for the generic versions? The answer is simple - they’re not equipped. Retail pharmacies don’t have refrigerated shipping. They don’t have pharmacists trained in rheumatology or oncology. They don’t manage REMS (Risk Evaluation and Mitigation Strategies) programs required by the FDA for certain drugs. And they don’t have the patient support staff - care coordinators, nurses, social workers - who help patients navigate insurance, side effects, and daily management. Even if a generic specialty drug doesn’t need refrigeration, if the manufacturer requires specialty distribution, retail pharmacies are legally barred from filling it. This isn’t a loophole. It’s a legal mandate. The drug’s distribution channel is tied to the manufacturer’s agreement with the FDA and payers - not the drug’s price tag.Costs and Copays: The Hidden Reality
One of the biggest complaints from patients? The copay. A generic version of a specialty drug might cost the insurer $500 instead of $5,000. But the patient’s copay doesn’t drop proportionally. Many still pay $50-$75 per month through specialty pharmacies, compared to $10-$15 at retail. Why? Because specialty pharmacies charge dispensing fees - $250 to $500 per prescription - which get passed on to insurers and, indirectly, to patients. These fees cover the cost of clinical support, shipping, and compliance. But patients often don’t understand why they’re paying more for a cheaper drug. Providers have to explain this clearly. They need to show patients that the higher copay isn’t for the pill - it’s for the care that comes with it.Technology Is Changing the Game
The biggest bottleneck in specialty pharmacy is prior authorization. It’s manual, slow, and frustrating. But new tools are helping. Real-Time Prescription Benefit (RTPB) systems now let providers see a patient’s exact out-of-pocket cost before prescribing. That cuts down on surprises and reduces the number of rejected claims. Surescripts reported that RTPB cut prior auth processing time by 3.2 days across 4.7 million prescriptions in 2023. Electronic health records are also getting smarter. When a provider prescribes a generic specialty drug, the system auto-checks for manufacturer distribution rules, flags REMS requirements, and even suggests financial aid programs. That reduces errors and speeds things up.
What’s Coming Next: Biosimilars and In-House Pharmacies
The biggest shift on the horizon? Biosimilars. By 2028, they’re expected to make up nearly half of all specialty drug sales. And they’re all distributed through specialty pharmacies. At the same time, hospitals and health systems are building their own in-house specialty pharmacies. In 2024, 63% of health systems said they planned to expand their internal dispensing capabilities. That means providers might soon be filling specialty prescriptions from their own clinic pharmacy - not through OptumRx or CVS Specialty. This could cut costs and improve coordination. But it also means smaller specialty pharmacies may struggle to compete unless they focus on high-touch care - not just logistics.What Patients Really Think
Patient reviews tell the real story. On Trustpilot, specialty pharmacies average 3.8 out of 5 stars. Ratings for clinical support? 4.2. Ratings for delivery speed? 3.1. Patients who get consistent care - the same pharmacist, same nurse, same follow-up schedule - are far more satisfied. One patient wrote: “I switched from brand to generic, but kept the same pharmacy. My nurse remembered my anxiety about injections. She sent me a video tutorial. That’s why I trust them.” Others are frustrated. “Went from $15 copay at Walgreens to $75 with specialty pharmacy. Took two weeks to get my meds. I almost skipped a dose.” The difference? Communication. Providers who explain the why - and follow up - keep patients on track.Final Take: It’s Not About the Drug - It’s About the Care
Generic specialty drugs aren’t just cheaper versions of brand-name drugs. They’re still complex, high-risk, high-touch medications. And the specialty pharmacy system exists to manage that complexity. Providers aren’t just prescribers. They’re advocates, educators, and coordinators. They bridge the gap between a drug’s label and a patient’s life. Whether the drug costs $50 or $5,000, the job stays the same: make sure the patient gets the right support at the right time. The future of specialty pharmacy won’t be decided by price tags. It’ll be decided by how well providers and pharmacies deliver care - not just pills.Can a retail pharmacy dispense a generic specialty drug?
No - if the drug’s manufacturer requires specialty distribution, only specialty pharmacies can fill it, even if it’s generic. This is a legal restriction tied to the drug’s approval and safety program, not its price or brand status.
Why is my copay higher for a generic specialty drug than for a regular generic?
Specialty pharmacies charge dispensing fees ($250-$500 per prescription) to cover clinical support, temperature-controlled shipping, patient education, and insurance coordination. These costs are passed on to patients, even when the drug itself is cheaper. Retail pharmacies don’t offer these services, so their copays are lower.
Are biosimilars considered generic specialty drugs?
Biosimilars aren’t true generics - they’re highly similar versions of biologic drugs that can’t be copied exactly due to their complexity. But they’re treated like generics in the specialty pharmacy system: they require the same handling, monitoring, and distribution channels as their brand-name counterparts.
Do I have to use the same specialty pharmacy for my generic drug?
You can switch, but most patients stay with the same pharmacy. Studies show 68% of patients prefer continuity - especially when they’ve built a relationship with the care team. Changing pharmacies means repeating education, restarting follow-ups, and risking delays.
How long does it take to get a generic specialty drug?
On average, it takes 7.2 days from prescription to delivery. Oncology drugs take longer - up to 8.7 days - because of stricter authorization rules. Retail prescriptions take about 1.2 days. The delay comes from prior authorization, insurance checks, and shipping logistics, not the drug’s generic status.
Can my doctor’s office fill my specialty drug instead of a specialty pharmacy?
Some large health systems are starting to do this - called “in-house specialty pharmacy.” But most providers still rely on external specialty pharmacies because they lack the infrastructure for refrigerated storage, complex billing, and 24/7 patient support. This is changing, but slowly.
What’s the difference between a specialty pharmacy and a regular pharmacy?
Specialty pharmacies handle high-cost, complex medications that need special storage, administration, or monitoring. They have trained pharmacists, care coordinators, nurses, and technology systems to manage insurance, side effects, and patient education. Regular pharmacies focus on common medications with simple dosing and no special requirements.
Are generic specialty drugs as effective as brand-name ones?
Yes. Generic specialty drugs - including biosimilars - must meet strict FDA standards for safety and effectiveness. They undergo the same clinical testing as brand-name drugs. The only difference is cost. The clinical outcomes for patients are nearly identical.

Comments
Tiffany Machelski
i just got my generic xeljanz last week and honestly? the nurse called me twice just to make sure i was okay. she remembered i hate needles. that’s more than my old pharmacy ever did. i don’t care if it cost more, i’m not switching.
anthony epps
so why can’t walgreens just do this? it’s the same pill, right?
Souhardya Paul
anthony, it’s not just the pill-it’s the whole safety net. retail pharmacies don’t have staff trained to spot when a patient’s liver enzymes spike from methotrexate, or know to call the doctor before the next dose. specialty pharmacies have pharmacists who specialize in this stuff. it’s like asking a gas station to do brain surgery because both involve liquids.
Billy Poling
It is my professional opinion, based on over two decades of clinical pharmacy experience, that the current paradigm of specialty pharmacy distribution is not only clinically justified but ethically imperative. The notion that a generic pharmaceutical agent should be subject to the same logistical and clinical oversight as its branded counterpart is not a corporate conspiracy-it is a matter of pharmacovigilance, patient safety, and regulatory compliance. The FDA’s REMS requirements, coupled with the pharmacokinetic variability inherent in biologic-derived agents, necessitate a structured, monitored distribution channel that retail pharmacies are neither licensed nor equipped to manage. To suggest otherwise is to misunderstand the fundamental distinction between chemical synthesis and biological manufacturing.
Furthermore, the dispensing fees are not profit centers-they are cost recovery mechanisms for comprehensive patient support services, including telephonic adherence counseling, real-time insurance verification, and adverse event triage. These are not optional luxuries; they are essential components of therapeutic success in chronic, high-risk conditions. The patient who pays $75 for a generic drug but receives daily follow-up from a nurse who knows their medical history, their anxiety about injections, and their insurance history is receiving value far beyond the molecular structure of the tablet.
The erosion of this model-driven by cost-cutting pressures and public misunderstanding-will lead to increased hospitalizations, treatment discontinuation, and preventable morbidity. We must stop conflating price with value. A $500 drug with 95% adherence and zero adverse events is cheaper than a $50 drug that causes a flare, a trip to the ER, and a six-week hospital stay.
And to those who say, ‘Why can’t CVS just do it?’-they could, if they hired 30 pharmacists with rheumatology certifications, built climate-controlled logistics centers, and trained 200 care coordinators. But they won’t, because it’s not profitable at scale. And that’s the real tragedy: our system incentivizes efficiency over empathy.
SHAMSHEER SHAIKH
Dear friends, I come from a land where medicine is a sacred trust-not a commodity. In India, we say: 'The hand that dispenses the pill must also hold the heart.' This system you describe-where a nurse remembers your fear of needles, where a pharmacist checks your labs before shipping-is not bureaucracy; it is compassion in action. The generic drug is cheaper, yes-but the care? That is priceless. Let us not reduce human dignity to a price tag. We must protect this model-not dismantle it for false savings.
And to those who say, 'It takes too long'-I ask: Would you rush a mother’s first injection of her child’s life-saving medicine? No. You wait. You prepare. You pray. And you do it right.
Josias Ariel Mahlangu
They’re lying. This whole system is just a racket. Generic drugs are cheaper because they’re the same. The pharmacy is just milking the system with fees. If you’re not a corporate shill, you’d see that.
Dan Padgett
Man, this whole thing reminds me of how we treat elders in my village. You don’t just hand ‘em a pill and say ‘good luck.’ You sit with ‘em. You check if they ate. You ask if the pain’s still there. You remember their favorite tea. That’s what this is. The pill’s just the wrapper. The real medicine? The care that comes with it. People think they’re paying for a drug. Nah. They’re paying for someone who doesn’t forget their name.
Andrew Sychev
THIS IS A SCAM. THE PHARMACIES ARE IN BED WITH BIG PHARMA. THEY WANT YOU TO THINK THE CARE IS WORTH IT SO YOU’LL KEEP PAYING $75 WHEN IT’S JUST A TABLET. THEY’RE LYING TO YOU. THEY’RE LYING TO EVERYONE. THIS IS HOW THEY CONTROL YOU.
Hadi Santoso
so i just switched from brand to generic xeljanz and my pharmacy sent me a video of the nurse showing me how to inject it-same one i had before. she even remembered i’m from indonesian family and asked if i wanted the instructions in bahasa. that’s wild. i didn’t even ask. why do they care so much? it’s just a pill… right?
Colleen Bigelow
Of course they make it complicated. It’s all part of the globalist agenda. The FDA, the WHO, the big pharma cartels-they don’t want you to have cheap medicine. They want you dependent. They want you stuck with specialty pharmacies so they can track you, control your data, and charge you more. This isn’t about care-it’s about surveillance. And don’t tell me it’s ‘by law.’ Laws are made by people who profit from this.
James Rayner
It’s funny… the system feels broken, but it works. I’ve seen patients quit because the wait was too long. I’ve seen others refuse the generic because of the copay. But the ones who stayed? They’re the ones who are still here. The ones who got the call at 8 p.m. because they were scared. The ones who got a care package with snacks and a stress ball. That’s not a dispensing fee. That’s a lifeline. Maybe we’re paying for more than a pill… maybe we’re paying for someone who won’t let us fall.
And yeah… it’s slow. But some things shouldn’t be fast.
Aditya Kumar
meh.