Understanding Spironolactone and Its Uses
Before we delve into the connection between spironolactone and irritable bowel syndrome (IBS), it is essential to understand what spironolactone is and how it is used. Spironolactone is a medication that belongs to a class of drugs called aldosterone antagonists or potassium-sparing diuretics. It is primarily prescribed to treat fluid retention, high blood pressure, and certain hormonal imbalances, such as those seen in polycystic ovary syndrome (PCOS) or acne.
Spironolactone works by blocking the action of the hormone aldosterone, which plays a role in regulating the balance of fluids and electrolytes in the body. By doing so, it helps the kidneys to remove excess water and sodium from the body, while retaining potassium. As such, the primary focus of spironolactone is on the renal and endocrine systems, but it is important to consider how it might affect other systems in the body, such as the digestive system and, more specifically, IBS.
Irritable Bowel Syndrome: A Brief Overview
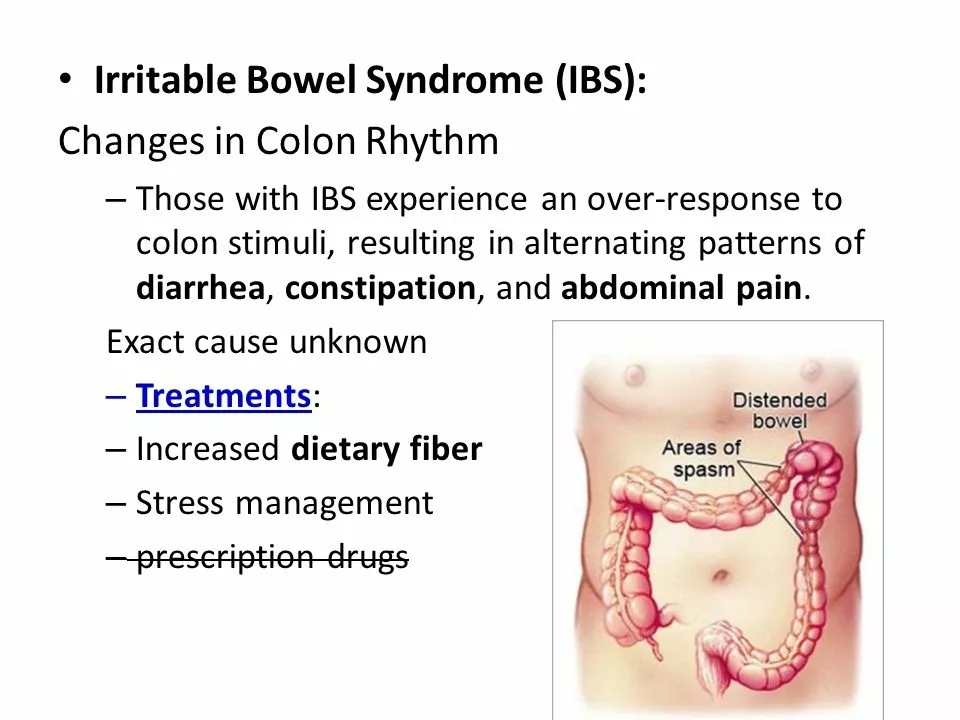
IBS is a common functional gastrointestinal disorder characterized by chronic abdominal pain, bloating, and altered bowel habits, such as constipation, diarrhea, or alternating between the two. The exact cause of IBS is still not entirely understood, but it is believed to be a result of a combination of factors, including gut-brain communication issues, heightened sensitivity to pain, gastrointestinal motility problems, and even changes in the gut microbiome.
IBS can be a challenging condition to manage, as there is no one-size-fits-all treatment. Instead, patients and healthcare providers must work together to develop a personalized approach to managing symptoms, which may include dietary modifications, stress management techniques, over-the-counter medications, and prescription drugs. In some cases, this may involve the use of medications like spironolactone.
Exploring the Connection Between Spironolactone and IBS
The connection between spironolactone and IBS is not a direct one, but rather an indirect association that arises from the medication's effects on the body. As a diuretic, spironolactone can cause increased urination and changes in fluid balance, which can potentially impact the digestive system and exacerbate IBS symptoms in some individuals.
For example, dehydration resulting from increased urination can lead to constipation, a common symptom of IBS. Additionally, electrolyte imbalances, particularly those involving potassium, can affect muscle function in the gastrointestinal tract, potentially causing cramping, bloating, or changes in bowel habits.
Managing IBS Symptoms While Taking Spironolactone
If you are taking spironolactone and experiencing IBS symptoms, it is important to discuss your concerns with your healthcare provider. They can help determine if the medication is contributing to your symptoms and suggest alternative treatments if necessary. However, there are also several strategies you can employ to help manage your IBS symptoms while taking spironolactone:
1. Stay hydrated by drinking plenty of water throughout the day. This can help counteract the dehydrating effects of spironolactone and prevent constipation.
2. Monitor your potassium levels and discuss any concerns with your healthcare provider. They may recommend dietary modifications or supplements to help maintain an appropriate balance.
3. Adopt a diet rich in fiber, which can help promote regular bowel movements and alleviate constipation.
4. Incorporate stress management techniques, such as yoga, meditation, or deep breathing exercises, into your daily routine, as stress can exacerbate IBS symptoms.
5. Engage in regular physical activity, which can help improve gastrointestinal motility and reduce stress.
Individual Differences and the Importance of Personalized Care
It is important to remember that each person's experience with IBS and spironolactone may differ, and what works for one individual may not work for another. Therefore, it is crucial to work closely with your healthcare provider to develop a personalized treatment plan that addresses your unique needs and concerns.
While there is no definitive link between spironolactone and IBS, it is essential to be aware of the potential impact the medication may have on your digestive system. By understanding the connection and employing strategies to manage IBS symptoms, you can better navigate your journey towards improved health and well-being.
Conclusion: The Connection Between Spironolactone and Irritable Bowel Syndrome
In conclusion, although there is no direct link between spironolactone and IBS, the medication's effects on fluid balance and electrolytes can potentially impact the digestive system and exacerbate IBS symptoms in some individuals. If you are taking spironolactone and experiencing IBS symptoms, it is important to consult with your healthcare provider to discuss your concerns and develop a personalized treatment plan. By staying informed and proactive in your healthcare, you can work towards effectively managing your IBS and maintaining your overall health and well-being.

Comments
Dipankar Kumar Mitra
Reading about spironolactone always makes me wonder how our bodies are such delicate machines, constantly juggling salts and hormones. The drug’s ability to spare potassium can feel like a quiet hero in the background, yet it can stir up turbulence in the gut for some people. If you’re already battling IBS, the extra fluid shifts might just tip the scales toward more cramping or constipation. It’s a reminder that every medication carries a ripple effect, touching systems we never expected. So, stay vigilant, track your symptoms, and keep the conversation open with your doctor.
Tracy Daniels
Great summary! 😊 Staying hydrated and monitoring potassium levels are indeed key strategies. I’d also suggest keeping a symptom diary to pinpoint any patterns related to the medication. It can be invaluable when discussing adjustments with your healthcare provider.
Hoyt Dawes
Honestly, this whole “stay hydrated” spiel feels like a generic health meme. If spironolactone truly worsens IBS, the real issue is the pharmaceutical industry’s rush to market without proper gut-focused trials.
Jeff Ceo
Look, we can’t dismiss the patient’s experience just because the side‑effects are “indirect.” The kidneys and gut are linked via blood volume, and any diuretic can alter motility. Doctors should take those reports seriously and consider dose tweaks or alternatives.
David Bui
Exactly, the connection isn’t a straight line but a web. The dehydration part can lead to harder stools, and low potassium can mess with muscle contractions in the intestine. It’s not rocket science, just basic physiology that many overlook.
Alex V
Oh sure, “just drink water” while a big pharma‑type script pushes pills that silently sabotage your gut. It’s almost like they want us to swap one problem for another, all while patting themselves on the back for “innovation”.
Robert Jackson
Stop trying to blame everything on the meds. Most folks get IBS from stress and diet, not some weird side effect.
Maricia Harris
Ugh, another “stay hydrated” reminder. Like we need that extra motivation when we’re already drowning in health tips. 🙄
Tara Timlin
Actually, hydration is crucial because spironolactone increases urine output, which can deplete fluids fast. Pairing water intake with electrolytes, especially potassium‑rich foods like bananas or avocado, can help maintain balance and reduce IBS flare‑ups.
Jean-Sébastien Dufresne
Listen up, folks! If you’re on spironolactone and your gut decides to rebel, it’s not just a coincidence. The drug shifts electrolytes-especially potassium-which directly influences smooth muscle function in your intestines. So, before you blame “just stress,” consider that the medication might be pulling the strings! 🚩
Patrick Nguyen
Adjusting dosage may alleviate the symptoms.
Patrick Bread
While it’s tempting to blame the pill for every tummy grumble, let’s not forget that lifestyle factors play a massive role. A balanced diet, regular exercise, and stress management often trump medication side‑effects in the long run.
Fiona Doherty
Right, as if a few extra steps could magically fix everything. Most of us can’t just overhaul our lives because a doctor says “try this.”
Neil Greer
Actually, small tweaks like adding a fiber supplement or a short walk after meals can make a noticeable difference without a total life rewrite.
Fionnuala O'Connor
Keep tracking your symptoms and share the data with your doctor it’ll help them fine‑tune your treatment plan.
Christopher MORRISSEY
When we examine the interplay between spironolactone and irritable bowel syndrome, it becomes evident that the human body operates as an intricate orchestra, each section influencing the other in subtle yet profound ways. The pharmacological action of spironolactone, primarily as an aldosterone antagonist, initiates a cascade of physiological changes that extend beyond the renin‑angiotensin‑aldosterone system. By promoting potassium retention and natriuresis, the medication inevitably alters the osmotic gradients that govern fluid distribution throughout the gastrointestinal tract. Such alterations can manifest as variations in bowel motility, potentially exacerbating the hypersensitivity that characterises IBS. Moreover, the diuretic effect may induce relative dehydration if fluid intake is not adequately calibrated, leading to firmer stools and heightened discomfort for those prone to constipation‑dominant IBS subtypes. Electrolyte shifts, particularly involving potassium, also affect smooth muscle contractility, which can result in cramping or irregular bowel patterns. It is crucial, therefore, for clinicians to adopt a holistic perspective, recognising that the benefits of spironolactone in managing conditions like hypertension or polycystic ovary syndrome must be weighed against its possible gastrointestinal repercussions. Patients, on their part, should be encouraged to maintain meticulous symptom logs, noting both the timing of medication intake and any corresponding digestive changes. This collaborative approach enables a nuanced assessment of causality and facilitates personalised therapeutic adjustments, such as dosage modulation or adjunctive dietary strategies. Incorporating fibre‑rich foods, adequate hydration, and regular physical activity can mitigate some of the adverse effects while preserving the primary therapeutic goals. In summary, the relationship between spironolactone and IBS is not a direct causal link but rather a complex interaction of fluid balance, electrolyte homeostasis, and gut motility. An informed, patient‑centred dialogue remains the cornerstone of optimal management.
Adam O'Rourke
Oh sure, just write a ten‑paragraph dissertation and the meds will magically stop messing with your gut-because that’s how medicine works, right? 🙄