Key Takeaways
- tympanites is abdominal swelling caused by gas, fluid, or both.
- FODMAPs are short‑chain carbs that ferment quickly and can trigger tympanites.
- The low‑FODMAP approach limits specific carbs while preserving nutrition.
- Tracking foods, fibre intake, and gut‑microbe health speeds up symptom relief.
- A personalized 7‑day meal plan can cut bloating by up to 60% within two weeks.
What Exactly Is Tympanites?
When you hear the word tympanites is a medical term for visible or palpable abdominal distension caused by excess gas, fluid, or a combination of both. It’s the same feeling many people call “bloating,” but tympanites is a clinical label doctors use when the swelling is pronounced enough to be measured or felt during an exam.
The condition isn’t a disease on its own; it’s a symptom that pops up in Irritable Bowel Syndrome (IBS), Small Intestinal Bacterial Overgrowth (SIBO), or even simple overeating. Knowing the root cause helps you treat the swelling instead of just masking it.
Why FODMAPs Matter
FODMAPs are a group of fermentable short‑chain carbohydrates - Fermentable Oligosaccharides, Disaccharides, Monosaccharides, And Polyols found in many everyday foods. Because they’re poorly absorbed in the small intestine, they travel to the colon where gut bacteria break them down, releasing gas and drawing water into the gut lumen. That combination creates the perfect storm for tympanites.
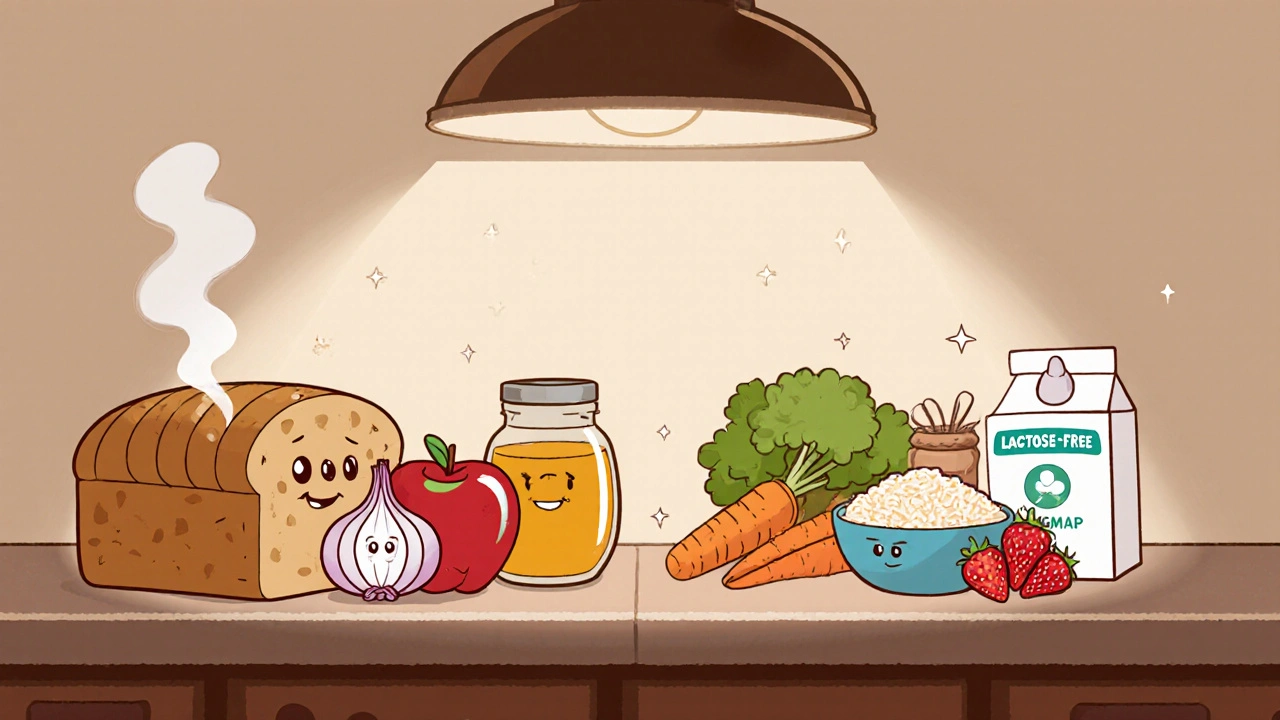
Common high‑FODMAP culprits include wheat, onions, garlic, apples, honey, and stone fruits. Even “healthy” foods like lentils and cauliflower can be troublemakers if you’re sensitive.
Low‑FODMAP Diet Basics
Low‑FODMAP diet is a structured elimination plan that removes high‑FODMAP foods for 4‑6 weeks, then gradually re‑introduces them to identify personal triggers. The goal isn’t permanent deprivation; it’s a discovery process that reveals which carbs your gut can tolerate.
The three phases are:
- Elimination: Cut out all high‑FODMAP items.
- Re‑challenge: Add one food group back every 3‑4 days while monitoring symptoms.
- Personalisation: Build a lifelong eating pattern that avoids only the problem foods.
During elimination, focus on low‑FODMAP staples like rice, quinoa, oats, carrots, zucchini, lactose‑free dairy, and firm tofu.
How Gut Microbiota Influences Bloating
Gut microbiota refers to the trillions of bacteria, fungi, and viruses living in your digestive tract that aid digestion, immune function, and nutrient synthesis. An imbalance-often called dysbiosis-exacerbates fermentation of FODMAPs, leading to more gas and fluid shift.
Boosting beneficial microbes with probiotics (live‑culture supplements or fermented foods) can reduce the severity of tympanites, especially when paired with a low‑FODMAP intake.
Step‑by‑Step: Implementing a Low‑FODMAP Plan
- Take a baseline food diary. Write down everything you eat for three days, noting bloating intensity on a 1‑10 scale.
- Identify high‑FODMAP red flags. Use the chart below to spot common triggers.
- Shop smart. Stick to a core list of low‑FODMAP items-rice, potatoes, carrots, cucumbers, eggs, and lactose‑free milk.
- Meal prep. Cook in batches so you always have a low‑FODMAP option on hand, avoiding the temptation to revert to high‑FODMAP comfort foods.
- Monitor and adjust. Continue the diary for the first two weeks. If symptoms drop below a 3, you’re likely on the right track.
- Re‑challenge gradually. Add one food group (e.g., garlic‑infused oil) for three days, then record any change.
- Finalize your personal list. Keep foods that cause a symptom rise >2 points out of your regular diet.
High‑FODMAP vs Low‑FODMAP Foods
| Category | High‑FODMAP (avoid) | Low‑FODMAP (safe) |
|---|---|---|
| Grains | Wheat, rye, barley | Rice, quinoa, gluten‑free oats |
| Fruits | Apples, pears, mango | Bananas (unripe), blueberries, strawberries |
| Vegetables | Onion, garlic, cauliflower | Carrots, zucchini, bell peppers |
| Dairy | Milk, soft cheese, yogurt | Lactose‑free milk, hard cheese, kefir (low‑FODMAP portion) |
| Legumes | Lentils, chickpeas, kidney beans | Canned lentils (drained), firm tofu |
| Sweeteners | Honey, high‑fructose corn syrup | Maple syrup, glucose syrup |

Sample 7‑Day Low‑FODMAP Meal Plan
Feel free to swap proteins or veggies, but keep portion sizes within low‑FODMAP limits (e.g., 1 cup cooked rice, 2 medium carrots).
- Day 1: Breakfast - Lactose‑free yogurt with strawberries; Lunch - Grilled chicken salad (lettuce, cucumber, olive oil); Dinner - Baked salmon, quinoa, sautéed zucchini.
- Day 2: Breakfast - Oatmeal (gluten‑free oats) with banana slices; Lunch - Rice‑paper rolls with shrimp, carrots, and mint; Dinner - Beef stir‑fry with bok choy and rice.
- Day 3: Breakfast - Scrambled eggs with spinach; Lunch - Quinoa bowl with roasted pumpkin, feta, and pine nuts; Dinner - Turkey meatballs, polenta, and roasted carrots.
- Day 4: Breakfast - Smoothie (lactose‑free milk, blueberries, chia seeds); Lunch - Tuna salad with lettuce, olives, and a drizzle of lemon oil; Dinner - Grilled pork chops, mashed potatoes (without milk), and green beans.
- Day 5: Breakfast - Rice cakes with peanut butter and sliced kiwi; Lunch - Chicken soup (clear broth, carrots, zucchini); Dinner - Baked cod, basmati rice, and roasted bell peppers.
- Day 6: Breakfast - Gluten‑free toast with avocado; Lunch - Lentil‑free hummus wrap (lettuce, cucumber, grilled tofu); Dinner - Lamb kebabs, quinoa tabbouleh (parsley, tomato, lemon).
- Day 7: Breakfast - Cottage cheese (lactose‑free) with pineapple; Lunch - Sushi bowl (sushi rice, smoked salmon, cucumber, seaweed); Dinner - Veggie pizza on a gluten‑free crust with mozzarella and tomatoes.
Checklist: Avoiding Common Pitfalls
- Don’t replace high‑FODMAP foods with large amounts of low‑FODMAP ones - balance is key.
- Watch hidden FODMAPs in packaged sauces, seasonings, and processed meats.
- Stay hydrated; low‑FODMAP diets can be low in fibre, so water helps prevent constipation.
- Re‑introduce foods slowly; a sudden re‑add can mask true tolerance levels.
- Consider a probiotic with strains Bifidobacterium infantis or Lactobacillus plantarum for added gut support.
Frequently Asked Questions
Is tympanites the same as normal bloating?
Both involve a swollen abdomen, but tympanites is clinically noticeable and often measurable, whereas everyday bloating may be mild and transient.
Can I follow a low‑FODMAP diet long‑term?
Yes, after the re‑challenge phase you keep only the foods that cause symptoms. The diet becomes personalized, not permanently restrictive.
Do all IBS patients have tympanites?
No. IBS can present with diarrhea, constipation, or pain without visible distension. Tympanites is just one possible manifestation.
What role does SIBO play in bloating?
Small Intestinal Bacterial Overgrowth (SIBO) is a condition where excessive bacteria colonise the small intestine, fermenting carbs that would normally be absorbed. This extra fermentation creates gas and water retention, often worsening tympanites.
Are probiotic supplements necessary?
Not always, but many people find strains like Bifidobacterium infantis reduce gas production. Choose a product with at least 5billion CFU and check for shelf‑stable packaging.


Comments
siddharth singh
If you’re dealing with tympanites, the first step is to pinpoint which carbs are inflaming your gut, because without a clear target the low‑FODMAP plan becomes a guesswork exercise. Start by logging every bite and beverage for three consecutive days, rating bloating on a scale of one to ten, and note any correlation with known high‑FODMAP culprits like wheat, onions, or apples. Once you have that baseline, eliminate all identified high‑FODMAP items for a solid four‑week window, but don’t panic-replace them with low‑FODMAP staples such as rice, quinoa, carrots, and lactose‑free dairy to keep calories and nutrients stable. During this elimination phase, focus on hydration; water helps offset the reduced fibre intake that often accompanies low‑FODMAP diets and prevents constipation, which can worsen abdominal distension. Incorporating a probiotic that contains Bifidobacterium infantis or Lactobacillus plantarum can also tilt the microbial balance toward gas‑reducing species, especially if you’ve had episodes of SIBO. When the four‑week mark arrives, re‑challenge each food group one at a time, waiting three to four days between introductions, and record any symptom spikes greater than two points on your bloating scale. If a food consistently triggers a rise, flag it as a personal trigger and keep it out of your regular rotation. Over time, you’ll compile a customized list that lets you enjoy a wide variety of meals without the dreaded balloon‑like feeling after each dinner. Remember that the goal isn’t permanent deprivation; it’s empowerment through knowledge, allowing you to make informed choices that keep tympanites at bay. Finally, keep an eye on hidden FODMAPs in processed sauces, dressings, and seasoning blends, because they’re easy to overlook and can sabotage your progress. By following this systematic approach, many folks report a reduction in bloating severity by up to sixty percent within two weeks, turning a chronic nuisance into a manageable aspect of daily life. Additionally, consider pairing low‑FODMAP meals with gentle physical activity like a short walk after eating, which can aid intestinal motility and reduce gas buildup. Avoid carbonated drinks during the trial, as the extra CO₂ can exacerbate abdominal pressure and mask the true effect of dietary changes. If you suspect an underlying condition such as SIBO, a breath test can provide diagnostic clarity and guide targeted antibiotic or herbal therapy. Keep the mindset flexible; occasional slip‑ups are normal, and the key is to return to the protocol rather than abandon it entirely. Sharing your progress with a supportive community, whether online or among friends, can also boost adherence and provide practical recipe ideas. Ultimately, the combination of diligent tracking, strategic elimination, gradual re‑introduction, and microbiome support forms a robust framework for taming tympanites and reclaiming comfort after meals.
Angela Green
Wow, fantastic summary-truly a comprehensive deep‑dive! Just a quick note for the grammar‑curious: when you’re talking about reducing carbs, the correct term is “fewer carbs,” not “less carbs,” because “carbs” is countable. Also, remember to hyphenate “low‑FODMAP” consistently; it improves readability and keeps the style crisp. Keep the energy up, and thanks for sharing such a helpful guide!
April Malley
Absolutely, thanks for the pointers-great catch!! I totally agree, the hyphenation does make a big difference, and using “fewer” keeps the sentence spot‑on. Let’s keep the conversation rolling, sharing more tips, and helping each other navigate the low‑FODMAP world together!!
Georgia Nightingale
In the grand theater of the human body, tympanites plays the role of an over‑inflated balloon yearning for release, a silent reminder that our internal chemistry mirrors the chaotic narratives we script in life. When fermentable carbs stage their fermentative fireworks within the colon, the resulting gas becomes a metaphor for suppressed thoughts, bubbling beneath the surface until the cosmos demands acknowledgment. Thus, a low‑FODMAP diet isn’t merely a culinary regimen; it is a ritual of self‑conciliation, a pact with one’s microbiome to restore equilibrium and silence the internal clamor. By methodically excising the culprits, we grant our gut the grace to breathe, echoing the philosophical principle that balance emerges from mindful omission. This drama, though subtle, underscores the profound interplay between diet, microbiota, and the psyche, inviting us to contemplate how even the smallest molecular exchanges can echo through the chambers of consciousness.
Viji Sulochana
i totally get what you’re saying, it’s like our belly’s got its own little drama club! just thought i’d add that sometimes just drinking more water can help the gas move out faster, even if the diet’s on point. keep it chill, everybody!
rohit kulkarni
Embarking upon a low‑FODMAP odyssey demands not only culinary vigilance but also an epistolary commitment to one’s own physiological narrative; each morsel becomes a stanza in the verse of gut harmony. By cataloguing intake with surgical precision-recording time, composition, and bloating intensity-you sculpt a dataset that rivals any scientific manuscript in its rigor. The ensuing elimination phase, akin to a chiaroscuro painting, strips away the cacophonous pigments of high‑FODMAP foods, revealing the subtle hues of tolerance that lie beneath. Re‑challenge, then, is the crescendo, a symphonic reintroduction of flavors calibrated to the metronome of symptomatology. Such disciplined choreography not only mitigates tympanites but also bestows upon the practitioner a profound appreciation for the alchemy of digestion.
RONEY AHAMED
You’ve got this!
emma but call me ulfi
I think sticking to the basics-simple grains, fresh veggies, and staying hydrated-can make a big difference without overcomplicating things.
George Gritzalas
Oh sure, because “low FODMAP” without the hyphen just screams professionalism, right? Let’s all ignore basic punctuation while we’re at it-what could possibly go wrong?
Jeremy Laporte
Hey, let’s keep things friendly-hyphens are handy, but we’re all learning, and the most important thing is that the diet works for you. If you need any simple tips or recipe ideas, just shout!