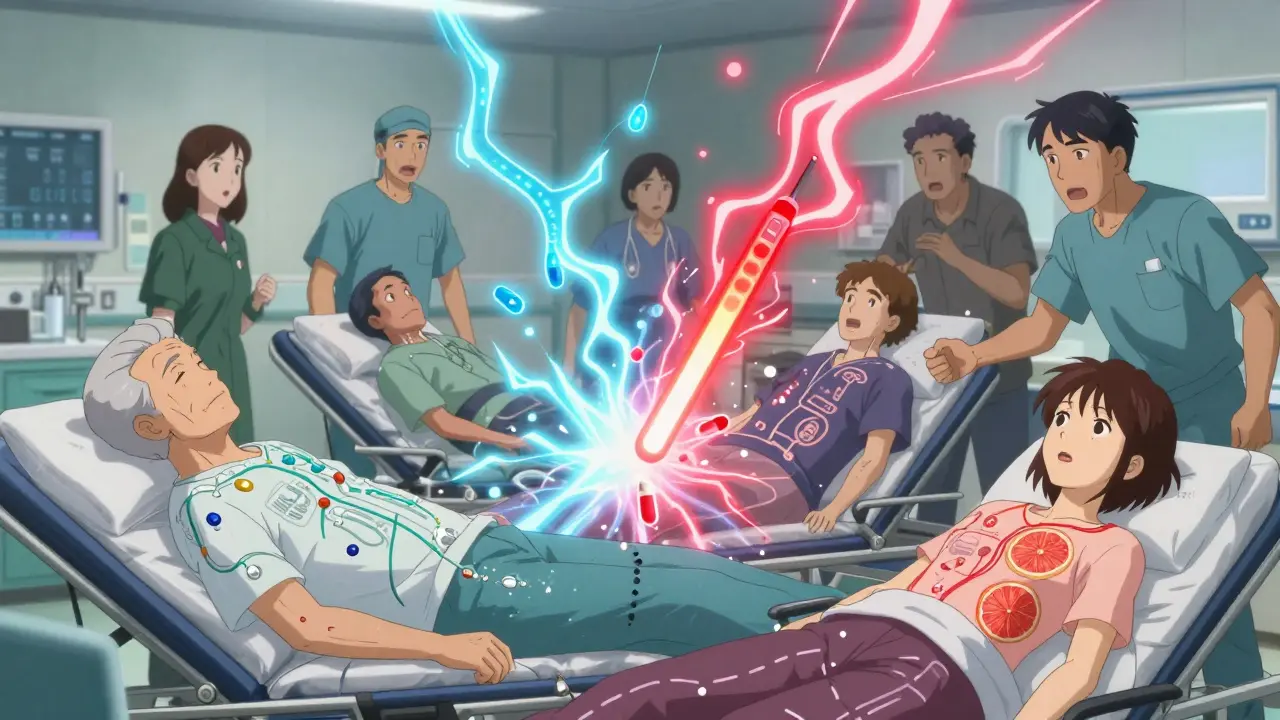
Every year, thousands of people end up in the hospital-not because their illness got worse, but because something they took to get better made things worse. This isn’t rare. It’s happening because of drug interactions. These aren’t just theoretical risks listed in fine print. They’re real, measurable, and often preventable. And if you or someone you care about is taking more than one medication, this isn’t something you can afford to ignore.
What Exactly Is a Drug Interaction?
A drug interaction happens when one substance changes how another substance works in your body. That substance could be another prescription drug, an over-the-counter pill, a vitamin, a herbal supplement, even your morning cup of grapefruit juice. It doesn’t have to be something you think of as "medicine."
There are three main types:
- Drug-drug interactions: When two or more medications affect each other. For example, taking the blood thinner warfarin with certain antibiotics can make your blood too thin, leading to dangerous bleeding.
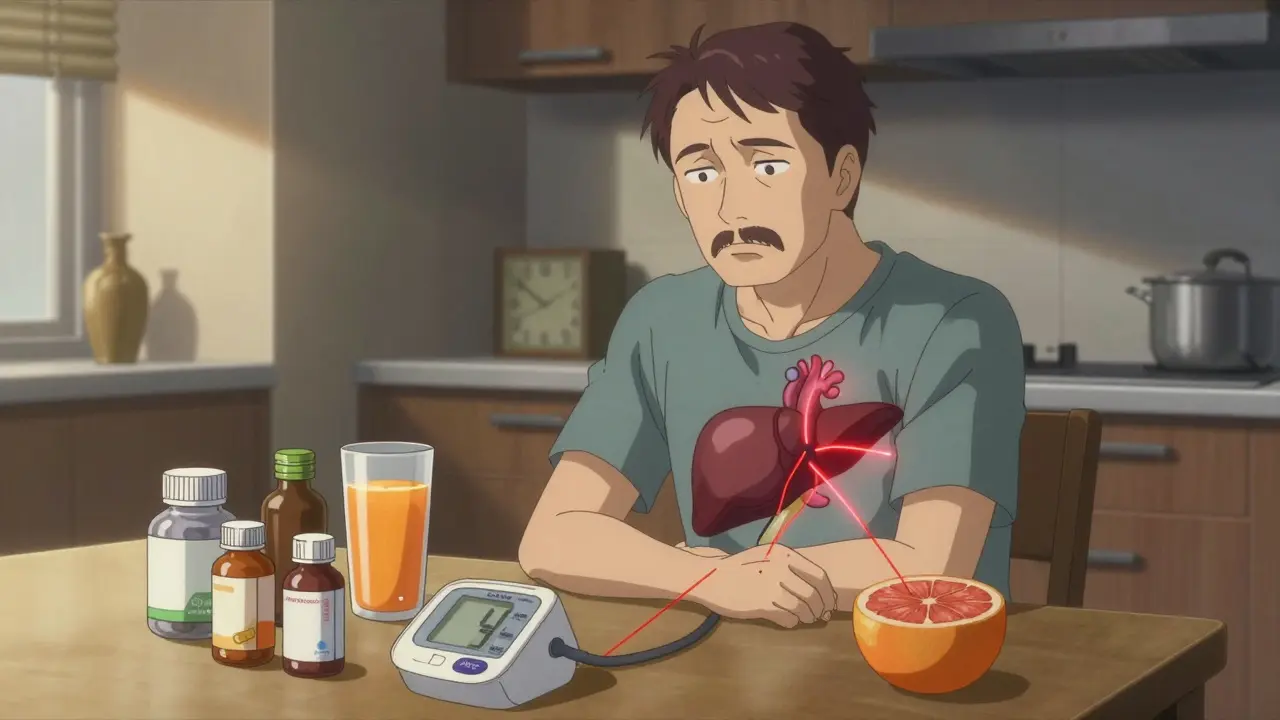
- Drug-food/drink interactions: When what you eat or drink changes how a drug is absorbed or broken down. Grapefruit juice is the most famous example-it can boost blood levels of some statins by up to 600%, raising the risk of muscle damage.
- Drug-condition interactions: When a health condition makes a drug riskier. For instance, taking certain blood pressure meds if you have kidney disease can push your kidneys into failure.
The body doesn’t treat every drug the same. It uses enzymes, especially a group called cytochrome P450 (CYP450), to break down medications. The enzyme CYP3A4 alone handles about half of all prescription drugs. If one drug blocks or speeds up this enzyme, it throws off the balance. Fluconazole (an antifungal) can slow down CYP3A4, causing simvastatin (a cholesterol drug) to build up in your blood to dangerous levels-sometimes 2,000% higher than normal. That’s not a typo. That’s enough to cause rhabdomyolysis, a condition where muscle tissue breaks down and can lead to kidney failure.
Why This Isn’t Just a "Minor" Problem
Drug interactions aren’t just a footnote in medical textbooks. They’re a leading cause of preventable harm. According to a 2022 study in JAMA Internal Medicine, serious drug interactions are responsible for over 106,000 deaths in the U.S. every year. That’s more than traffic accidents. It’s also behind about 6.5% of all hospital admissions. Think about that: nearly 7 out of every 100 people admitted to the hospital are there because of a drug interaction.
The financial cost? Around $30 billion annually in avoidable healthcare spending. That includes emergency room visits, hospital stays, and long-term care. The total cost of all medication-related problems? Over $528 billion per year in the U.S. alone, according to the Agency for Healthcare Research and Quality.
And it’s not just about big, dramatic events. Sometimes the harm is subtle: a medication stops working, your blood pressure doesn’t drop, your thyroid levels stay off, or you feel unusually tired. These are all signs something’s off-and it might be an interaction.
Who’s Most at Risk?
You might think this only affects older people. And yes, they’re the most vulnerable. The average person over 65 takes 4.7 prescription medications daily. That’s not unusual. But with each added drug, the risk of a bad interaction grows. Older adults experience drug interactions at three times the rate of younger people. A 2022 AARP survey found that 42% of Medicare beneficiaries over 65 had at least one harmful interaction.
But it’s not just seniors. People with five or more chronic conditions are at high risk too. Nearly 70% of them have at least one significant interaction. And it’s not just about quantity-it’s about the drugs themselves. Warfarin, for example, has over 600 known interactions. Digoxin? More than 300. Levothyroxine? Over 200. If you’re on any of these, you’re playing with a loaded gun.
Even healthy people can be at risk. Grapefruit juice affects more than 85 drugs. A single glass can do damage. And it’s not just grapefruit-pomegranate, Seville oranges, and even some herbal teas can cause similar problems.
What Makes an Interaction Dangerous?
Not all interactions are created equal. Some are minor-like a slight delay in absorption. Others are life-threatening. Here’s how they’re generally ranked:
- Contraindicated: Never combine. These are absolute no-gos. For example, taking sildenafil (Viagra) with nitroglycerin can drop blood pressure to deadly levels.
- Significant: Requires monitoring or dose changes. Warfarin and antibiotics fall here. Your INR levels need to be checked often.
- Minor: Low risk, often just an inconvenience. Like taking an antacid with an antibiotic-might reduce absorption a little, but not dangerous.
The problem? Many patients don’t know which category their interaction falls into. A 2022 study in Drug Safety found that major drug databases disagreed on the severity of interactions in nearly 4 out of 10 cases. So even if you check an app, you might get conflicting advice.
The Silent Epidemic in Polypharmacy
Modern medicine has given us incredible tools. But it’s also created a new problem: polypharmacy. That’s when someone takes five or more medications at once. It’s common. The average person takes 1.5 prescription drugs and 1.2 over-the-counter products simultaneously, according to the National Center for Health Statistics.
But here’s the catch: doctors rarely talk to each other. A patient might see a cardiologist, a rheumatologist, a neurologist, and a primary care doctor-all prescribing different drugs. None of them know what the others have prescribed. A 2022 study in the New England Journal of Medicine found that 34% of patients discharged from hospitals had at least one undocumented interaction risk because of fragmented care.
And it’s not just doctors. Pharmacists are often the last line of defense. The American Society of Health-System Pharmacists reports they resolve 3.5 million drug-related problems every year. Of those, 22% are drug interactions. That means for every five problems they fix, one is a dangerous combination no one else caught.
Real Stories, Real Consequences
On Reddit’s r/pharmacy community, over 140 people shared stories of warfarin interactions after starting antibiotics. One woman took amoxicillin for a sinus infection and ended up in the ER with internal bleeding. Another man took fluconazole for a yeast infection and had a stroke because his INR shot up overnight.
Then there’s the grapefruit story. A man in his 60s took simvastatin for years with no issues. Then he started drinking grapefruit juice every morning. Within 48 hours, he was hospitalized with rhabdomyolysis. His muscle enzymes were off the charts. He spent weeks in the hospital. He never drank grapefruit juice again.
But there are good stories too. One patient said her pharmacist caught that her new antidepressant interacted dangerously with her blood pressure med. She never took the first pill. The pharmacist called her doctor. They switched prescriptions. She’s fine now.

How to Protect Yourself
Knowledge isn’t power here-it’s protection. Here’s what actually works:
- Keep a full list of everything you take. Include prescriptions, OTC meds, vitamins, supplements, and even herbal teas. Write down the dose and how often you take it.
- Use one pharmacy. That way, the pharmacist can track everything you’re on and flag risks before you even leave the counter.
- Ask about interactions every time you get a new prescription. Don’t assume your doctor knows. Ask: "Could this interact with anything I’m already taking?"
- Check your meds with reliable tools. Use the FDA-approved GoodRx Drug Interaction Checker or Medscape’s free tool. Avoid consumer apps that don’t list severity levels.
- Time your doses. If a supplement like calcium or iron interacts with your thyroid med, take them at least 2 hours apart.
- Know your high-risk drugs. Warfarin, digoxin, levothyroxine, statins, and certain antidepressants are on the danger list. If you’re on one of these, be extra careful.
And if you’re over 65? Make sure your doctor uses the Beers Criteria-a list of 54 high-risk drug combinations for older adults. Using it can cut adverse events by 27%.
The Future: Personalized Safety
There’s hope on the horizon. The FDA launched the Drug Interaction Knowledgebase (DIKB) in 2023-a machine-readable system with over 12,000 validated interactions. AI tools like IBM Watson are now scanning millions of clinical notes to find patterns humans miss.
By 2026, pharmacogenomic testing (checking your genes to see how you metabolize drugs) could become standard for high-risk medications. If your body breaks down a drug too slowly or too fast, your doctor can adjust the dose before you even take it.
But until then, the system is still broken. Pharmaceutical companies often underreport interactions in clinical trials. The FDA admits only 25% of serious interactions are caught before a drug hits the market. Most are discovered after people start taking them.
That means your safety doesn’t rely on the system. It relies on you.
Final Thought
Medication safety isn’t about avoiding drugs. It’s about using them wisely. A pill that saves your life can also kill you-if it’s not used correctly. Drug interactions aren’t scary because they’re rare. They’re scary because they’re common, predictable, and preventable. You don’t need to be a doctor to protect yourself. You just need to be informed, curious, and willing to ask the hard questions.
Can drug interactions happen with over-the-counter medications?
Yes, absolutely. Many people assume OTC drugs are harmless, but that’s not true. Ibuprofen can interfere with blood pressure meds. Antacids can block absorption of antibiotics and thyroid medication. Even common supplements like St. John’s Wort can reduce the effectiveness of birth control, antidepressants, and heart medications. Always check interactions-even for pills you buy without a prescription.
Is grapefruit juice really that dangerous?
Yes, for certain medications. Grapefruit contains compounds that block an enzyme in the gut (CYP3A4) that normally breaks down drugs. This causes more of the drug to enter your bloodstream. For statins like simvastatin or atorvastatin, this can raise levels by 300-600%, increasing the risk of muscle damage and kidney failure. Even one glass can have a lasting effect-up to 72 hours. If you’re on a statin, check with your pharmacist. Alternatives like orange juice are usually safe.
Why do some drug interactions only show up after years of use?
Because your body changes. Your liver and kidneys don’t work the same at 65 as they did at 35. Your diet changes. You start taking new meds. A drug that was fine for five years might suddenly become dangerous when you add a new supplement or develop a kidney issue. Interactions aren’t always immediate-they can build up over time. That’s why regular medication reviews are critical.
Can herbal supplements cause drug interactions?
Definitely. St. John’s Wort is one of the worst offenders-it can make birth control, antidepressants, HIV meds, and transplant drugs ineffective. Garlic supplements can thin your blood, which is risky if you’re on warfarin. Ginkgo biloba can increase bleeding risk. Even ginger and turmeric can interfere with blood sugar control and blood thinners. Just because something is "natural" doesn’t mean it’s safe with your meds.
How can I tell if I’m having a drug interaction?
Watch for sudden changes: unexplained fatigue, dizziness, unusual bruising or bleeding, muscle pain, confusion, or a medication that suddenly stops working. If you’ve recently started a new drug, supplement, or changed your diet, and you feel off, an interaction could be the cause. Don’t wait-call your doctor or pharmacist right away.

Comments
Sarah Barrett
It’s staggering how many lives are quietly unraveling because of something as simple as grapefruit juice and a statin. I never realized how much my body was doing behind the scenes-enzymes, metabolic pathways, silent negotiations between chemicals I didn’t even know existed. It’s like finding out your car’s engine has a hidden fuse box that only one mechanic in the state understands. And yet, we treat medications like candy. I keep a laminated card in my wallet with every pill, supplement, and even the herbal tea I drink. It’s not paranoia. It’s precision.
Erica Banatao Darilag
i just found out my mom took kava root with her blood pressure med and almost had a stroke. i didnt even know kava was a thing. why do people think herbal = safe? its like saying wild mushrooms are fine because they grow in nature. my mom is fine now but i dont trust anythng anymore. i write evrything down on a napkin now. lol.
Michael Page
The human body is not a pharmacological sandbox. It is a dynamic, self-regulating system of biochemical feedback loops that evolved over millions of years-not designed by a committee of pharmaceutical executives. When we introduce synthetic molecules into this system without understanding their full kinetic profile, we are not treating illness-we are conducting uncontrolled experiments on ourselves. The fact that we accept this as normal speaks volumes about the epistemological bankruptcy of modern medicine.
Charlotte Dacre
So let me get this straight-we’ve got AI scanning clinical notes, FDA databases, and pharmacogenomics on the horizon… but we still can’t stop people from mixing warfarin with antibiotics because they didn’t read the label? I mean, if you can’t be bothered to ask your pharmacist, maybe you shouldn’t be allowed to own a pill bottle. Just sayin’.
Kapil Verma
India has been managing polypharmacy for decades without your fancy apps. We have Ayurveda, homeopathy, and common sense. In my village, we mix turmeric with ghee and take it with our medicines. No interaction. No hospital. No American overreaction. You people treat every pill like a bomb. We treat health like a lifestyle. You need to learn from us, not the FDA.
Mandeep Singh
You think grapefruit is bad? Try taking levothyroxine with calcium supplements and then wonder why your TSH is still 8.5 after six months. I’ve been on thyroid meds since I was 19. I’ve seen doctors who didn’t know the difference between T3 and T4. My pharmacist had to call three specialists before they realized I was taking my thyroid pill with my morning smoothie. I’ve lost 17 pounds, gained 12 pounds of anxiety, and cried in a CVS parking lot because no one asked me about my protein powder. This isn’t medicine. It’s a lottery.
Betty Kirby
Let’s be real. The system is rigged. Drug companies don’t test for interactions because they don’t want to know. They want you on five drugs, not one. And don’t even get me started on how pharmacies are understaffed. I’ve had pharmacists hand me a bottle without even glancing at my list. And then they act shocked when I end up in the ER. It’s not your fault. It’s not your doctor’s fault. It’s a broken machine. And we’re all just rats in the wheel.
Josiah Demara
People who don’t track their meds are a public health hazard. I’ve seen patients die because they took St. John’s Wort with their antidepressant and didn’t think it mattered. You think ‘natural’ means ‘safe’? That’s the same logic that led to the opioid crisis. You don’t get to opt out of responsibility because you’re too lazy to Google. This isn’t a suggestion. It’s a survival protocol. If you’re on more than three meds and you haven’t sat down with a pharmacist in the last six months, you’re one bad interaction away from a coroner’s report.
Kaye Alcaraz
One pharmacy. One list. One question. That’s all it takes. I’ve coached dozens of elderly patients through this. You don’t need to be a scientist. You just need to be consistent. Write it down. Bring it. Ask. Repeat. It’s not complicated. It’s just inconvenient. And convenience is the enemy of safety. You don’t have to be perfect. Just present. That’s enough.
Esha Pathak
Think about it-your body is a temple, but we treat it like a vending machine. Push a button, get a pill. No thought. No reflection. No gratitude. We’ve forgotten that medicine is not a transaction. It’s a conversation. Between you, your enzymes, your liver, your kidneys, and the universe of molecules you’ve invited in. When you ignore that, you’re not just risking side effects-you’re disrespecting the very architecture of life. 🌿
Mike Hammer
My grandpa took 11 pills a day. We used to joke he was a walking pharmacy. Then he started drinking cranberry juice with his blood thinner. One morning, he woke up with a black eye he didn’t remember getting. Turned out his INR was 8. He spent three weeks in the hospital. Now he only takes what he absolutely needs. And he drinks orange juice. Simple. Smart. Lifesaving.
Daniel Dover
Use one pharmacy. Done.